
Parents Need Time, Not Deadlines, After Fetal Diagnoses
Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
Blog Post
Cancer patients in the U.S. must contend with more than just their disease. They have to get smart about catching billing errors and launching appeals when their insurance plan refuses to cover care. And then they must decide if some of their treatment is unaffordable.
The U.S. health system stands out for making the patient “responsible for acquiring the knowledge and skills needed to effectively use those goods or services and to ensure they’re of high quality,” said University of Pennsylvania School of Social Policy & Practice Assistant Professor and LDI Senior Fellow Meredith Doherty. “Health care is largely treated as a consumer product, so the onus is on the consumer.”
That burden has been shown to interrupt access to care in many areas of medicine. And now a study from Doherty and her team presents the first look at the effect of these administrative demands on cancer care. The team examined survey responses from 510 patients and survivors collected by a national nonprofit patient advocacy group. Of the patients and survivors, 55% were on Medicare, Medicaid, or both, while 37% had commercial insurance.
Paperwork raised the odds by nearly 50% for patients to delay care or fail to follow through with appointments, tests, and prescriptions. Young adults and Black patients reported more challenges with paperwork than other groups. The more tasks patients had to deal with, the more likely they were to experience cost-related delays.
Patients said cost concerns drove their engagement in administrative tasks. They looked at costs before filling a prescription, getting lab tests or scans, or agreeing to a recommended treatment.
Patients also spent time asking insurance companies for help understanding coverage or appealing denials.
Billing errors were a particular sore spot. “For those who do engage, there’s frustration, exhaustion, and I think a sense of alienation,” said Doherty. “If you send me a bill erroneously and can’t help me correct it, you’re showing me you don’t care about me.”
Research suggests that a large proportion of patients with cancer are affected by care-related financial harm, or financial toxicity, and that cost concerns can make them skip aspects of care.
Doherty’s team found a similar pattern. One-third of those surveyed said they sometimes postponed care or skipped it to reduce costs.
This is the first study to find a link between administrative tasks and cost-related delays in cancer care. The findings highlight that patients with cancer face challenges created by the system that is designed to give life-saving care.
While the motivation between paperwork and care delays remains unknown, easing that burden could improve quality, value, and patient experience. Possible solutions include patient education interventions, adapting hospital-based financial navigation programs, and policy changes that ease interactions among patients, physicians, and payers.
Doherty hopes this work will spur conversations to begin simplifying the system. “I think we’re at a place now where we may want to quantify how much improvement in access and other outcomes we might see if we alleviated some of these administrative burdens,” she said.
The study, “Administrative Burden Associated with Cost-Related Delays in Care in U.S. Cancer Patients,” was published in Cancer Epidemiology, Biomarkers & Prevention in August 2023. Authors include Meredith Doherty, Bridgette Thom, and Daniel S. Gardner.


Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector
Research Brief: Less Than 1% of Clinical Practices Provide 80% of Outpatient Services for Dually Eligible Individuals

New Findings Highlight the Value of 12-Month Eligibility in Reducing Care Gaps and Paperwork Burdens
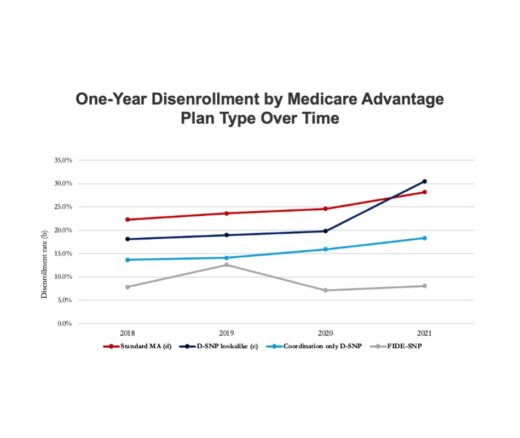
Chart of the Day: Fully Integrated D-SNPs Kept These Vulnerable Patients Enrolled, a New Study Finds

Democrats Must Go Beyond Reversing Trump-Era Cuts With a New Strategy to Streamline Coverage, Reduce Waste, and Expand Access to Medicaid