
Medicare’s Hidden Fix for High Drug Costs
Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print
Health Care Access & Coverage | Health Equity
[Original post: George Maliha, Michael Adelberg, Krisda H. Chaiyachati, During COVID-19, Minding The Access Gap: Addressing Both The Digital And Transportation Divides To Improve Outcomes, Health Affairs Blog, November 12, 2021. https://www.healthaffairs.org/do/10.1377/hblog20211105.682777/full/?utm_medium=social&utm_source=twitter&utm_campaign=blog&utm_content=chaiyachati Copyright ©2021 Health Affairs by Project HOPE – The People-to-People Health Foundation, Inc.]
Prompted by concerns that some in-person care was too dangerous during the 2020 COVID-19 pandemic, the US health care sector accelerated telehealth’s expansion. While telehealth has improved access to many outpatient services, marginalized patients—rural, poor, older, and minority patients—may not have benefitted equally from telehealth’s expansion. This stems, in part, from the “digital divide”—differential access to personal technology or broadband connectivity that results from historic disparities in economic means or educational attainment.
If the digital divide is not addressed, ongoing and broader implementation of telehealth could exacerbate inequities in health and health care outcomes. Understandably, policy makers and health systems have been focused on equity initiatives to narrow the digital divide: expanding broadband access, distributing digital devices, and deploying digital health navigators or community health workers.
While laudable, initiatives designed to address the digital divide may be focused on a shrinking and unpredictable slice of care delivered in the US. As of May 2021, telehealth’s share of all outpatient claims trended below 5 percent compared to its pandemic peak of 13 percent. The reasons for this downward trend are likely multifactorial: Providers and patients may prefer in-person interactions, and there may be clinical indications for in-person examination, testing, or vaccinations. Furthermore, telehealth regulations and payment reforms were broadly enacted using emergency authorizations with planned expiration dates in late 2021, leading to uncertainty over telehealth’s regulatory and payment future.
Telehealth is arguably here to stay, but its future remains in flux. This time of uncertainty, however, should not cause health care providers, payers, and policy makers to lose sight of telehealth’s underlying potential to improve access to care. Indeed, as today’s pendulum swings back toward in-person, office-based care, marginalized patients are stuck squarely in a gap: losing potential access gains from telehealth while re-encountering pre-pandemic barriers to in-person care. During this transitory moment, the health care sector should invest in post-COVID-19 infrastructure that is more responsive to the access needs of all patients than the pre-pandemic system; the digital divide must be addressed but so must the “transportation divide.”
Transportation is an analogue to telehealth—a medium to connect patients to providers. Despite the existence of non-emergency medical transportation (NEMT) programs, transportation barriers have been neglected and understudied. For instance, even though Medicaid has provided a NEMT benefit since 1965 and Congress in 2020 mandated that state programs provide NEMT, approximately 5 percent of Medicaid enrollees routinely report they delayed care because of transportation challenges. Outside of Medicaid, surveys of underserved populations highlight how transportation was a barrier 10 percent to 50 percent of the time, correlating with geography, disability, insurance status, or clinical condition. Yet, beyond the Medicare Advantage program where transportation has grown rapidly as an optional, supplemental benefit, the health care sector has not applied the same degree of energy nor innovation toward narrowing the transportation divide as it has applied toward narrowing the digital divide.
Ignoring the transportation divide could prove to be perilous for marginalized populations. We propose four solutions to guide the path forward. First, we need to shift our view of NEMT from a regulatory mandate to be met to a potential tool for meeting a desired end—better health and well-being for patients. Otherwise, debates about NEMT will continue to narrowly revolve around the administration of the program—poor service delivery, limited ride availabilities, and documentation challenges that have led to poor patient experiences, inefficiency, and low-use rates. Similarly, research has focused on isolated, service-delivery benefits of transportation, such as reducing missed office-based appointments or facilitating efficient discharge from inpatient wards.
While measuring NEMT performance in these areas is important, focusing only on these metrics misses the larger point. NEMT should be viewed more expansively, designed, and evaluated as a health care intervention with potential health outcome gains. If it does not meet these goals, it should be redesigned.
In this light, NEMT should not simply benefit the Medicaid or Medicare population but should be expanded for individuals in need within all insurance programs, public or private, and arguably the uninsured. We should focus on identifying clinical conditions in which in-person care provides the best possible outcome relative to virtual care modalities such as telehealth. For example, the Biden administration’s partnership with Uber and Lyft to offer discounted rides for people who used them to travel to and from a COVID-19 vaccination site could motivate upwards of 12 percent of unvaccinated individuals to receive the vaccine. Transportation could be a friction-reducing intervention that connects patients to care that has high public health or population health value, such as vaccinations, preventive care, or behavioral health care.
Second, the federal government, states, and other payers should modernize their NEMT services to facilitate future improvements in productivity, costs, and service so that patients view it as a useful and desired benefit; otherwise, we will not be able to fully understand its full potential to improve outcomes. Localities and private insurers already have key data about enrolled beneficiaries necessary to develop a system to provide patients with a vehicle that meets their accessibility needs at the correct time at a convenient location. More than 10 states have turned to transportation network companies that enhance traditional NEMT services with rideshare networks.
Going further, state programs and private insurers should partner to share resources, using GPS, ride-tracking, driver ratings, and other technologies to improve customer satisfaction and ensure compliance with public accountability rules. The federal government can help with initial investments or reconfiguring program rules to facilitate such partnerships, as startup costs pose barriers to entry for new providers and would-be innovators.
Third, greater cross-sector collaborations could occur, or at minimum stakeholders could align efforts. The Federal Communications Commission has collaborated with the Department of Health and Human Services to narrow the digital divide. Similar collaborations within the transportation sector can be strengthened. Already, many local transportation providers—in states such as Iowa and Vermont—depend on Medicaid NEMT dollars to help support more general transportation services. It is important to remember that many of the most vulnerable have disabilities or communication barriers, or reside in rural areas outside Lyft and Uber service areas. Investing in preexisting transportation networks to deepen ties with disabled individuals, non-English speakers, and underserved areas would lessen duplication of efforts and help support more robust local transportation networks and infrastructure.
Finally, those engaged in digital-divide advocacy and those engaged in transportation-divide advocacy should find ways to collaborate. The purpose of both groups is to improve access to care, and both will be judged on their ability to improve health outcomes. If we can shrink the digital divide for marginalized patients while at the same time reducing transportation barriers, marginalized patients can have nagging social risk factors lifted, allowing patients and their providers to focus on improving care, not whether patients can access it in the first place.
Many of the innovations of the past year—telehealth expansion, licensing liberalization, payment reform, and equity initiatives—show us that access-related reforms are possible. As the nation eventually emerges from the COVID-19 pandemic and the telehealth revolution equilibrates, we should have the foresight to use transportation as a complementary tool to enhance health care access and not leave patients stuck between two divides.

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools

Pandemic-Era Medicare Flexibilities Have Proven Effective, Popular, and Safe

A 2024 Study Showing How Even Small Copays Reduce PrEP Use Fueled Media, Legal, and Advocacy Efforts As Courts Weighed a Case Threatening No-Cost Preventive Care for Millions
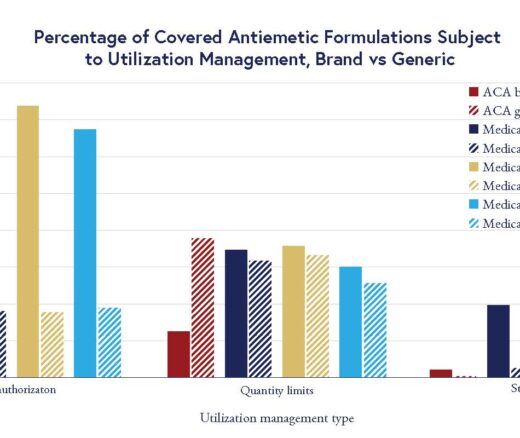
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior