Blog Post
National Shifts in Outpatient Care for Patients With Cirrhosis
Sustained Telemedicine Use During Pandemic

As the U.S. enters the tenth month of the COVID-19 pandemic, it is hard to imagine a time when telemedicine was not a mainstay of health care delivery, particularly in the care of vulnerable patients. However, few studies have examined the scale of how outpatient care has changed at the national level, and whether the changes have been sustained beyond the early months of the pandemic. In our recent study in Hepatology Communications, we found that telemedicine use for outpatient hepatology care in the Veterans Health Administration (VHA) not only dramatically increased during the early months, but has continued at similar levels as the pandemic progresses.
Using data from nearly 130,000 VHA patients with cirrhosis, we identified all outpatient hepatology visits completed across the United States from January 1, 2020 through August 11, 2020. We classified these visits as “in-person” or “telemedicine.”
Telemedicine visits were infrequent in the pre-pandemic period. However, they increased rapidly early in the pandemic, while in-person visits declined dramatically. These shifts were observed across the entire United States, with a >300% increase in telemedicine visits from baseline. Importantly, the total number of outpatient visits remained generally similar throughout—suggesting that these patients had few lapses in access to outpatient specialty care despite the transition to telemedicine (Figure 1).
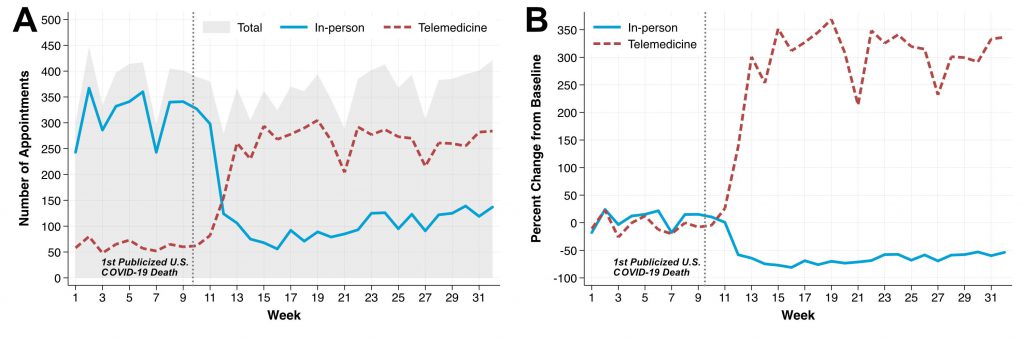
The proportion of outpatient visits conducted via telemedicine increased during the pandemic for nearly all states. For example, most states in the pre-COVID period had fewer than 20% of all visits performed through telemedicine, whereas by late April 2020 and into the summer, most states had >60% of all visits conducted through telemedicine (Figure 2). While in-person visits began to increase later in 2020, outpatient telemedicine visits remained relatively constant through the study period.
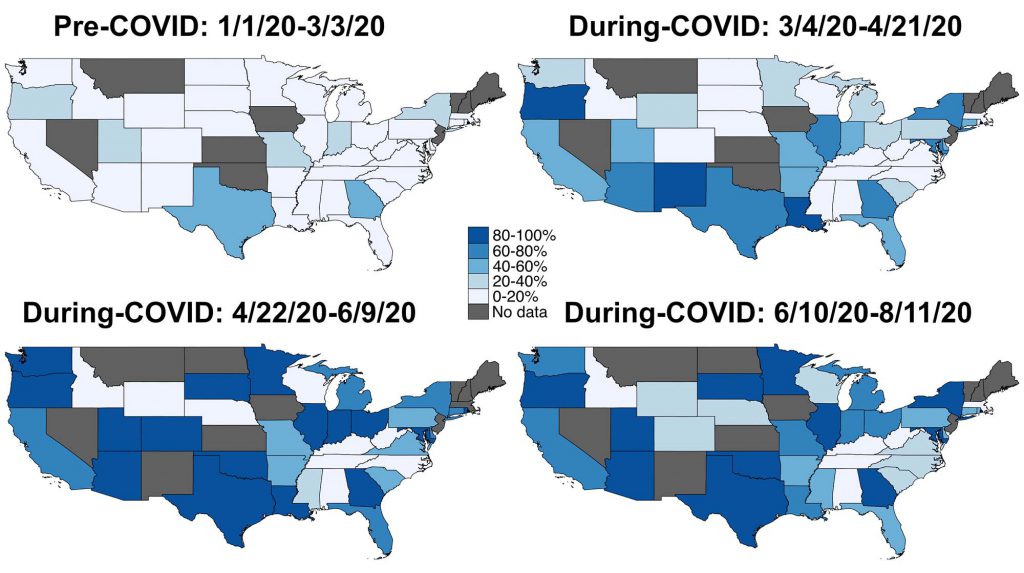
Additionally, Black patients and patients 70 years and over were less likely to receive telemedicine in the pre-pandemic period, but these demographic differences disappeared during the pandemic. This may reflect the impact of targeted initiatives in the VHA system to expand telemedicine access to certain patient populations with limited telemedicine capabilities.
While our findings suggest that outpatient telemedicine use has continued beyond the early months of the pandemic, it remains to be seen if expansion in telemedicine-based infrastructure will lead to more permanent use of remote care. Further research should also consider how shifts in care delivery have affected quality of care, including whether demographic disparities in outcomes persist despite improved telemedicine access overall.
This study was supported by a COVID-19 Rapid Response Grant from Penn LDI. In response to the pandemic, this grant supports LDI Senior and Associate Fellow projects that address urgent questions related to population health, health care delivery, or health policy during the pandemic. Learn more about LDI’s response to COVID-19 here.
The study, Major Shifts in Outpatient Cirrhosis Care Delivery Attributable to the COVID‐19 Pandemic: A National Cohort Study, was first published online in Hepatology Communications in October 2020. Authors include Nadim Mahmud, David S. Goldberg, David E. Kaplan, and Marina Serper.