
New Rules for Methadone Doses at Home Did Not Increase Overdoses
More Flexible Methadone Take-Home Policy Improved Patient Autonomy
Substance Use Disorder
Blog Post
The epidemic of opioid use and overdose has a little-known impact on another national health crisis—U.S. maternal mortality, which is the worst of any high-income country. A remedy for these two issues is the subject of a new study by LDI Associate Fellows Xi Wang and Douglas Strane and Senior Fellows Zachary Meisel and Meredith Matone.
Drug overdose is a leading cause of death in the year after giving birth. Opioid-related diagnoses at hospital deliveries jumped more than five times between 1999 and 2017, from 1.5 to 8.2 per 1,000.
The good news, Wang said, is that we have evidence-based, Food and Drug Administration (FDA)-approved treatments for opioid use disorder (OUD) for birthing individuals: methadone and buprenorphine. Her study focused on buprenorphine because of evidence that it has lower risks for newborns than methadone when taken during pregnancy. Buprenorphine is also the only medication for OUD that can be prescribed from a physician’s office instead of a treatment program.
Only 1 in 3 eligible people in the study, who all had private insurance, received this guideline-recommended treatment, however. Wang said, “We asked ‘why don’t pregnant and postpartum people have adequate and equitable access to a treatment that we know is effective?’”
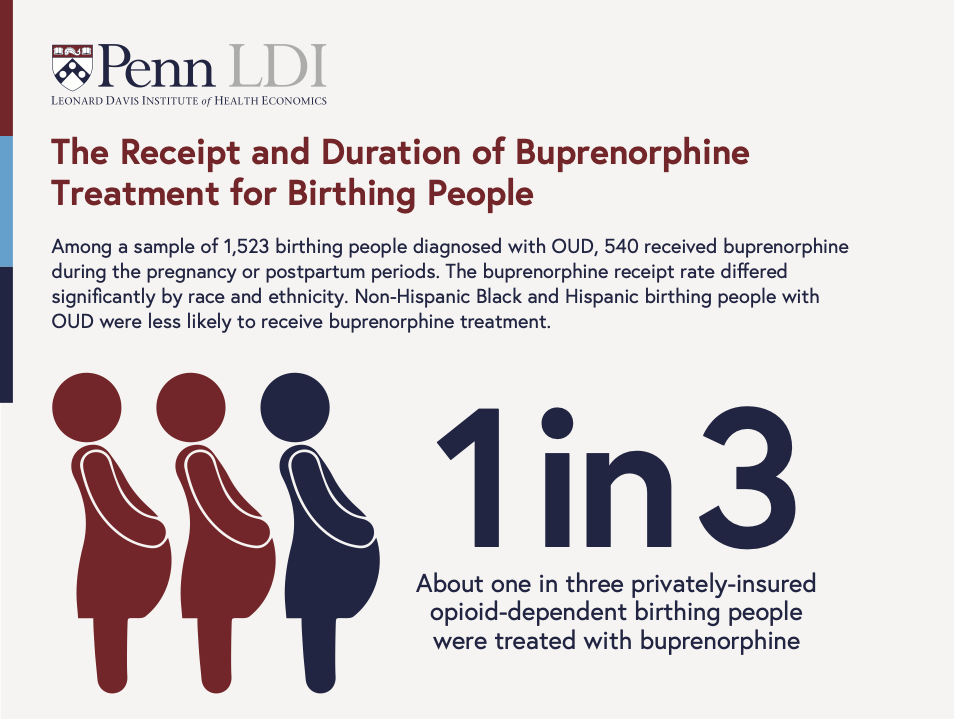
The researchers studied a group of 1,523 people with OUD who gave birth from 2017 to 2020. In this national sample, about 79% of opioid-dependent birthing people identified as non-Hispanic white, 11% as non-Hispanic Black, and about 9% identified as Hispanic. Many had co-occurring mental or behavioral health conditions such as depression or bipolar disorder in addition to OUD.
Overall, only 36% of people who might benefit from buprenorphine received it. Treatment differed by race and ethnicity: Only 29% of Black and 23% of Hispanic individuals with OUD received buprenorphine in the period surrounding a pregnancy.
Where patients lived also mattered. Some states have programs that support substance use treatment during pregnancy. Other states criminalize opioid use during pregnancy or define it as child abuse or neglect, which can result in loss of custody. These policies may make patients hesitant about seeking care for OUD and clinicians wary about providing it.
Wang and colleagues found that living in a state with punitive policies was linked to the lowest buprenorphine use—under 23%—compared to 43% in states with the least restrictive policies. Other research shows that from 2000 to 2015, these punitive policies became more common.
Based on previous studies on retention in treatment, Wang and colleagues determined how many patients used buprenorphine for at least six months. From prescription fills, only half of patients who received buprenorphine stayed in treatment for six months or longer. One-third of patients had an interruption in treatment during that time.
A promising result was that buprenorphine treatment increased from 30% in 2017 to 43% in 2020. If treatment barriers are lowered, Wang and colleagues’ study on inequities in buprenorphine treatment could support tailored policies and programs for reducing pregnancy and postpartum deaths from opioids. Their recommendations include:
Wang is now studying whether the same barriers to pregnancy and postpartum buprenorphine treatment confront people with public insurance, such as Medicaid. She is currently funded by LDI to study OUD treatment access by determining travel times to the nearest facility with a substance use disorder treatment program that accepts people who are pregnant or postpartum. Other work by Wang and colleagues includes talking with patients, medical professionals, and program administrators about structural and social factors that might increase buprenorphine treatment during and after pregnancy.
“OUD in pregnancy is a complex issue,” Wang said. “No one group can solve the problem, so the ideal is multifactorial solutions that include comprehensive prenatal and postpartum care, coordinated addiction and mental health treatment services, and policies and social safety net programs that support families.”
The study, “Receipt and Duration of Buprenorphine Treatment During Pregnancy and Postpartum Periods in a National Privately-Insured Cohort,” was published on November 10, 2023 in Drug and Alcohol Dependence Reports. Authors include Xi Wang, Zachary Meisel, Katherine Kellom, Jennifer Whitaker, Douglas Strane, Anyun Chatterjee, Rebecka Rosenquist, and Meredith Matone.


More Flexible Methadone Take-Home Policy Improved Patient Autonomy

Pediatricians’ Suggestions for Health Care Providers, Institutions, and Policymakers

Pain Is Hard to Predict, and a Cheap Disposal Kit Offers a Solution

New Geographic Trends Raise Questions About the Future of Behavioral Health Services

This Model Is Cheaper And Easier To Use Than The ER, LDI Fellow Argues In New Op-Ed