Health Care Access & Coverage | Improving Care for Older Adults
News
Philadelphia/Penn Collaboration Expands Use of Evidence-Based Mental Health Treatments
ALACRITY Retreat Details Partnership's Latest Implementation Science Successes and Challenges in City's Clinics
 |
||
| Photos: Hoag Levins
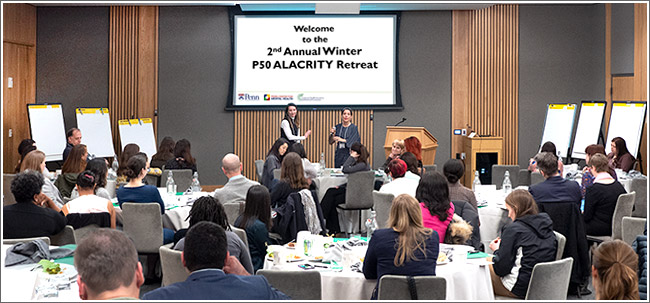
Addressing the Second Annual Winter Retreat of the University of Pennsylvania ALACRITY research center are Rebecca Stewart, PhD, and Rinad Beidas, PhD, both of the Penn Center for Mental Health (CMH) and the Leonard Davis Institute of Health Economics (LDI). Aimed at improving care throughout Philadelphia’s network of community mental health clinics, ALACRITY is a NIMH-funded research collaboration of CMH and Penn’s Center for Health Incentives and Behavioral Economics (CHIBE). (Click image for larger) Thirty years ago, in the wake of the state’s deinstitutionalization of mental health patients, the Philadelphia Department of Health and Human Services set out to build the country’s largest city-controlled managed behavioral health care organization. It also entered into a collaborative relationship with the University of Pennsylvania to gain the scientific expertise of Penn’s many behavioral health experts. Today, with a $1.6 billion annual budget, the City’s Department of Behavioral Health and Intellectual disAbility Services (DBHIDS) is the primary source of mental health care for Philadelphia’s 750,000 Medicaid recipients, 160,000 of whom receive various kinds of services annually. Seventy seven percent of these Medicaid patients are either African American or Hispanic. ALACRITY is the latest chapter in the 30-year DBHIDS/Penn collaboration, nationally viewed as one of the most unique municipal/academic partnerships of its kind. |
||
   |
||
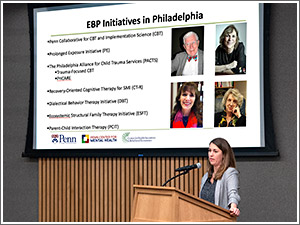
| ALACRITY and DBHIDS are working together to increase clinicians’ use of the latest evidence-based practices (EPBs) throughout Philadelphia’s network of community mental health clinics. From 2013 to 2017, the DBHIDS/Penn implementation efforts increased clinicians’ use of EBP treatments six percent. “That six percent is significant because it’s the foothold that we needed to begin moving the system forward,” said DBHIDS Deputy Commissioner for Strategic Planning and Innovation Roland Lamb (above, left). “Our relationship with Penn’s scientists has been essential to what we’re trying to do.” Above, right, welcoming Penn health services research scientists and city health professionals to the one-day retreat, was Rinad Beidas, PhD, Director of the Penn Implementation Science Center (PISCE), and co-principal investigator of the ALACRITY Center. “Everything we’re doing centers around our shared mission of leveraging science to provide the very best mental health care we can to Philadelphia citizens, and striving to be a national and international leader in how to deliver public behavioral health care.” | ||
  |
||
| “Our mission is to radically transform mental health care for individuals with psychiatric disorders by leveraging behavioral economics, participatory design, and implementation science to get the things we know work out into communities faster,” David Mandell (above, left) told the audience. Mandell, ScD, is the Director of the Penn Center for Mental Health, an LDI Senior Fellow, and co-principal investigator of the ALACRITY Center. “We’ve funded a lot of pilot grants during the course of ALACRITY so far. Many of those have turned into additional NIH-funded proposals or grants. I’m particularly excited about the training grants that have been submitted because one part of our mission is to create the next generation of researchers who are doing this work.” Above, right, the third ALACRITY co-principal investigator, Alison Buttenheim, PhD, MBA, synopsized the day’s individual group discussions about lessons learned so far in the ALACRITY project. She noted a surprising number of participants recommended adding a more vigorous communications component. “There were lots of ideas about marketing, data visualization, and infographics; a lot of interest in ‘can you show us this in a new way that could get providers excited about evidence-based approaches?’,” said Buttenheim, Associate Director of the Penn Center for Health Incentives and Behavioral Economics (CHIBE) and an LDI Senior Fellow. | ||
  |
||
| Rebecca Stewart, PhD (above, left), a licensed clinical psychologist, Assistant Professor at the Penn Center for Mental Health (CMH), and LDI Senior Fellow, specializes in research focused on “non-adopters,” or health care organizations and clinicians that haven’t switched to new evidence-based treatment methods. In 2013, DBHIDS launched the Evidence-Based Practice & Innovation Center (EPIC) to centralize and coordinate its effort to implement evidence-based practice throughout the city’s network of mental health providers. Stewart presented a “Curve of Adoption” chart showing EPIC’s initiative has gained significant traction in 40 percent of the 211 providers. Above, right, Carrie Comeau, LCSW, EPIC Director, spoke of that progress. “I’ve seen the difference in how the entire system is talking about EBP now; that’s a huge shift in the level of awareness and understanding from how it was before,” she said. “We have an opportunity in the immediate term to build upon what we have started, and to think about being accountable and community-driven. A goal for this year is to establish a community advisory board.” | ||
  |
||
| “We look forward to taking what we learned over the past 13 years and using it to inform our next steps,” said Chris Tjoa, MD, Chief Medical Officer of DBHIDS’ Community Behavioral Health (CBH) division. “We’re asking, ‘what are the best ways to run our training programs so that clinicians come out and are supported in delivering EBP treatment, and how can we better focus on infrastructure development?’.” Above, right, speaker Torrey Creed, PhD, is directly involved in implementing EBPs in clinical organizations that haven’t previously used them. One of the most surprising findings she reported was the results of surveys of the patients themselves. “One hundred percent of them said they had found EBP by luck,” Creed said. “They had never heard about it before, didn’t hear about it at intake, but when they got into the therapist’s office, the therapist said, ‘Hey, I have this thing I know how to do that I think could really help you. It’s called evidence-based practice.'” | ||
  |
||
| Exchanging insights and observations (above, left) during the “Lessons Learned” group discussions are (l to r) Sosunmolu Shoyinka, MD, Chief Medical Officer DBHIDS; Molly Candon, PhD, Research Assistant Professor of Psychiatry at the Penn Center for Mental Health, Lecturer in Health Care Management at the Wharton School, and LDI Senior Fellow; and Katelin Hoskins, MSN, MBE, a Robert Wood Johnson Foundation Future of Nursing Scholar and doctoral student at the Penn School of Nursing, and an LDI Associate Fellow. Above, right, in nearby table discussions, are Courtney Benjamin Wolk, PhD (hands), Assistant Professor of Psychiatry at Perelman and LDI Senior Fellow, and Molly Davis, PhD (green blouse), Postdoctoral Fellow at the Penn Center for Mental Health. | ||
  |
||
| Above, left, engaged in a lively “Planning for the Future” group discussion session were (l to r) Christina Johnson, Clinical Research Coordinator at the Penn Center for Mental Health; Kelly Zentgraf, MS, a Project Manager at the Center for Mental Health; Alison Buttenheim, PhD, MBA; Thomas Mackie, PhD, MPH, Assistant Professor, Rutgers School of Public Health; Tamra Williams, PhD, Deputy Chief Clinical Officer, Community Behavioral Health; Tamar Klaiman, PhD, MPH, Adjunct Professor of Health Policy and Public Health, University of the Sciences; Courtney Benjamin Wolk, PhD; and Molly Davis, PhD. Above, right, leading another table discussion are Adina Lieberman, MPH, Manager of Research Projects at the Penn Center for Mental Health (yellow dress) and Kimberly Arnold, PhD, Postdoctoral Fellow at the Penn Center for Mental Health (gray sweater). To the right of Arnold: Mary Phan, Clinical Research Coordinator, Penn Center for Mental Health; Mia Everett, MD, Medical Director for Children’s Services at CBH; Kit Wislocki, Clinical Research Coordinator, Penn Center for Mental Health; and Torrey Creed, PhD, Assistant Professor of Psychiatry at the Perelman School of Medicine. | ||
  |
||
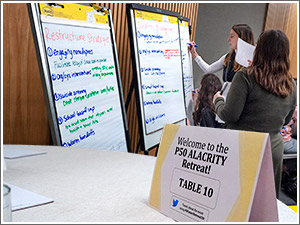
| The “Planning for the Future” group sessions resulted in ideas charted out (above, left) in six areas: Restructure Strategies, Quality Management, Policy Context, Finance, Plan Strategies, and Education. Above, right, David Mandell leads the final Retreat session in a review and open discussion of those dozens of ideas for how to further support and spread the use of EBP’s throughout Philadelphia’s network of Community Mental Health clinics. | ||