
Patients Face New Barriers for GLP-1 Drugs Like Wegovy and Ozempic
Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools
Blog Post
In 1972, Congress dramatically expanded the Medicare program by extending its coverage to most individuals with end-stage renal disease (ESRD). In ESRD, the final, permanent stage of chronic kidney disease, the kidneys can no longer function independently, and so survival depends on dialysis or kidney transplantation. In our recent article in the Journal of American Society of Nephrology, we argue that a recent U.S. Supreme Court decision could threaten the delivery of life-sustaining dialysis to this population.
Although Medicare now covers the majority of ESRD care in the United States, dialysis centers depend on the higher reimbursements from private insurance. To balance costs to Medicare while ensuring profit margins for dialysis facilities, Congress enacted the Medicare Secondary Payer Act in 1981, which enabled ESRD patients to remain on their private insurance for up to 30 months before transitioning to Medicare. The Act mandated two protections for ESRD patients: during the 30-month period, private insurance plans could not (1) “differentiate” between patients with ESRD and patients without ESRD, nor (2) “take into account” their eligibility for Medicare.
Any development that reduces these protections risks shifting more reimbursements to Medicare, which could affect the financial viability—and by extension, the delivery—of dialysis in this country.
Yet when the Supreme Court considered the meaning of these two protections for ESRD patients last term, it decided that the Medicare Secondary Payer Act did not prevent private insurance plans from providing minimal or unfavorable coverage for dialysis, as long as such limits applied to all beneficiaries equally. In the case, Marietta Memorial Hospital Employee Health Benefit Plan v. DaVita, Inc., a major dialysis provider had sued Marietta Health Benefit Plan for treating all dialysis providers as out-of-network and limiting payments to dialysis centers to 87.5% of the Medicare rate.
Marietta Health Benefit Plan’s practice increased deductibles and copays for reimbursements for patients with ESRD. As a result, such coverage decisions could increase the likelihood that patients with ESRD will transfer to Medicare more quickly than Congress envisioned, depriving dialysis units of revenue from private insurance. This could, in turn, lead dialysis units to consolidate in densely-populated areas to increase patient counts and achieve better economies of scale. Dialysis access barriers would thus intensify, particularly for patients living in rural areas.
To prevent such access barriers, we provide three possible policy response:
Regardless of the path forward, policymakers must reconcile the conflicting priorities of ensuring ESRD patients remain cared for safely and effectively, protecting Medicare’s future viability, and maintaining affordable coverage for non-ESRD patients. This recent Supreme Court decision likely makes that task much harder.
The perspective, “Ensuring Equitable Access to Dialysis: The Medicare Secondary Payer Act in Marietta Memorial Hospital Employee Health Benefit Plan v. DaVita, Inc.,” was published in the August 2022 issue of the Journal of American Society of Nephrology. Authors include George Maliha, Joel Glickman, and Matthew McCoy.



Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools

A 2024 Study Showing How Even Small Copays Reduce PrEP Use Fueled Media, Legal, and Advocacy Efforts As Courts Weighed a Case Threatening No-Cost Preventive Care for Millions
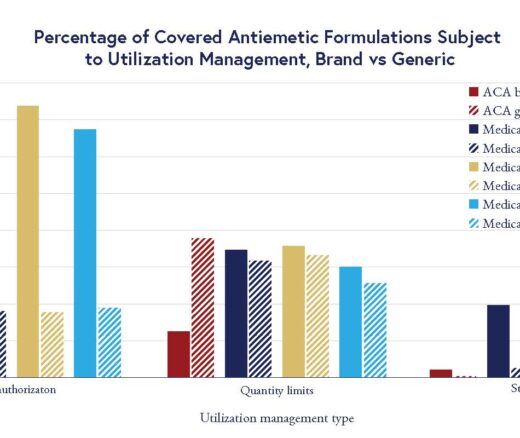
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities