
Why Work Requirements Won’t Work for Medicaid
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector
Blog Post

Can a reliable ride to the hospital improve your health? In the world of health care, where every moment is crucial, missing out on essential medical care simply because of transportation can be life-threatening. This is the reality for the 3.6 million Americans who live with health-related transportation insecurity, according to the American Hospital Association’s guide, “Transportation and the Role of Hospitals.”
LDI Senior Fellow Marina Serper, working with Harvard Medical School Assistant Professor Nneka Ufere and colleagues, studied how transportation affects the lives of the 4.5 million Americans with chronic liver disease (CLD) in the United States. In their study in Hepatology Communications, the authors looked at the relationship between care-related transportation insecurity and financial security, self-reported health status, work productivity, outpatient and acute health care utilization, and mortality.
About 6% of the 152,836 adults with CLD surveyed reported experiencing care-related transportation insecurity. These individuals faced a cascade of challenges, from financial strains to compromised health outcomes.
The study discovered some intriguing correlations. Transportation insecurity was linked to increased chances of cost-related drug nonadherence, food insecurity, and a decline in self-reported health status. The authors also found an association between transportation-related anxiety and increased health care use and mortality.
According to the authors, transportation insecurity is a critical risk factor that should be screened for. They also suggest expanding insurance benefits to include medical transport to appointments, along with supporting broadband internet to improve access to telemedicine.
To learn more about the study, we asked Drs. Serper and Ufere a series of questions.
Serper: When we encounter patients with transportation issues, we ask our social workers to address whether there are extended social supports they can leverage for rides and help them set up medical transportation. For patients who are being evaluated or waitlisted for liver transplantation, this is especially important as they have urgent appointments they cannot miss. However, many patients are not part of the transplant pathway and lack sufficient support. These cases are more challenging. We do supplement with telemedicine visits and home care in situations where people are homebound, but this still leaves us with a vulnerable population.
A different Penn study offering Lyft rides showed low uptake among a vulnerable population. This suggests patients may have other more pressing social needs; addressing only transportation barriers may not be enough.
Ufere: As part of our study conceptual framework, we believed that there were associations between transportation insecurity and other social risk factors such as food and financial insecurity, as well as self-reported health status and work-productivity (due to the lack of access to transportation generally). We found that the CLD population experiencing transportation insecurity is particularly socially vulnerable due to co-occurring financial and food insecurity. Patients with social risk factors, particularly those with financial insecurity, often have to make difficult decisions on how to best use their limited household income which can lead to tradeoffs as they make decisions to pay for their basic needs (food, housing) versus health care (transportation costs to get there, paying for medications, etc.).
Serper: The study indicates that individuals living in poverty, with functional limitations, and those who are under- or uninsured, have a higher health care-related transportation burden.
Serper: I am working on home-based physical activity and nutrition programs for patients with cirrhosis and those who have received a liver transplantation. The goal is to extend more care at home and to provide remote visit monitoring. This study on a home-based physical activity program that increased steps with an incentive payment is an example.
Ufere: Future research can expand upon this study by employing thoroughly validated instruments to evaluate the multifaceted factors contributing to health care-related transportation insecurity. This research could focus on prospective studies involving well-characterized cohorts of patients with chronic diseases, particularly those undergoing evaluations such as liver transplantation for cirrhosis. By investigating the relationship between transportation insecurity and both pre- and post-transplant health outcomes, further insights can be gained into the impact of transportation barriers on health care utilization and overall health outcomes in individuals with chronic diseases.
Serper: Insurance providers could provide medical transportation to appointments, expand the use of telemedicine, and bolster broadband internet access so that the internet can reach populations without internet access. However, it is important to note that telehealth can exacerbate health care disparities among patients with low digital literacy and low access to technology.
National organizations have a role to play. For example, the American Association for the Study of Liver Diseases (AASLD) recently released quality measures to improve liver transplant quality, including access. Dr. Ufere and I both authored this guidance, along with a team of doctors from across the country. Efforts like these can help medical practices and transplant programs measure barriers in access to care, some of which may be related to transportation.
Ufere: Similar to what Dr. Serper mentioned, policymakers should consider including non-emergency medical transportation (NEMT) as an insurance benefit for all Medicare enrollees (currently only available as a supplemental benefit in those with eligible Medicare Advantage [MA] plans) and removing restrictions that limit the use of NEMT services (i.e., prior authorization) for Medicaid and Medicare enrollees. In addition, national paid leave policies would greatly benefit both working patients with CLD and their family caregivers on whom they often rely upon for support to and from medical care.
The study, “Health-Care Related Transportation Insecurity is Associated With Adverse Health Outcomes Among Adults With Chronic Liver Disease,” was published in January 2024 in Hepatology Communications. Authors include Nneka Ufere, Carlos Lago-Hernandez, Alysa Alejandro-Soto, Tiana Walker, Lucinda Li, Kimberly Schoener, Eileen Keegan, Carolina Gonzalez, Emily Bethea, Siddharth Singh, Areej El-Jawahri, Lauren Nephew, Patricia Jones, and Marina Serper.


They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector
Research Brief: Less Than 1% of Clinical Practices Provide 80% of Outpatient Services for Dually Eligible Individuals

New Findings Highlight the Value of 12-Month Eligibility in Reducing Care Gaps and Paperwork Burdens
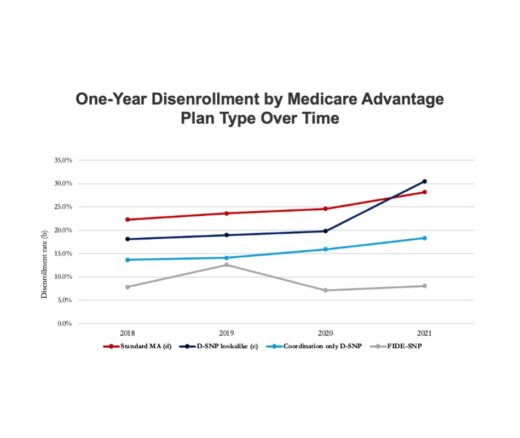
Chart of the Day: Fully Integrated D-SNPs Kept These Vulnerable Patients Enrolled, a New Study Finds

Democrats Must Go Beyond Reversing Trump-Era Cuts With a New Strategy to Streamline Coverage, Reduce Waste, and Expand Access to Medicaid

A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike