
Over 500 U.S. Hospitals Have Stopped Delivering Babies Since 2010
A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike
Health Care Access & Coverage
Blog Post

Pneumonia is one of the leading causes of hospitalization among adults. With the perpetual push toward value-based care and alternative payment models that incentivize providers to improve care and lower costs, pneumonia’s prevalence makes it a good candidate for episode‐based care models. As an acute infection, pneumonia may be a more natural fit for episode-based payment than hospital admissions for exacerbations of chronic conditions, such as heart failure. But in practice it’s not that simple, and there are barriers to payment reform for pneumonia care.
While pneumonia is common, it often presents with other conditions that can make designing a successful payment bundle difficult. In a new study titled “Pneumonia is Not Just Pneumonia,” LDI Executive Director Rachel M. Werner, Senior Fellow Amol S. Navathe, and colleague Jessica T. Lee find that comorbid conditions associated with pneumonia complicate the payment landscape for patients and providers.
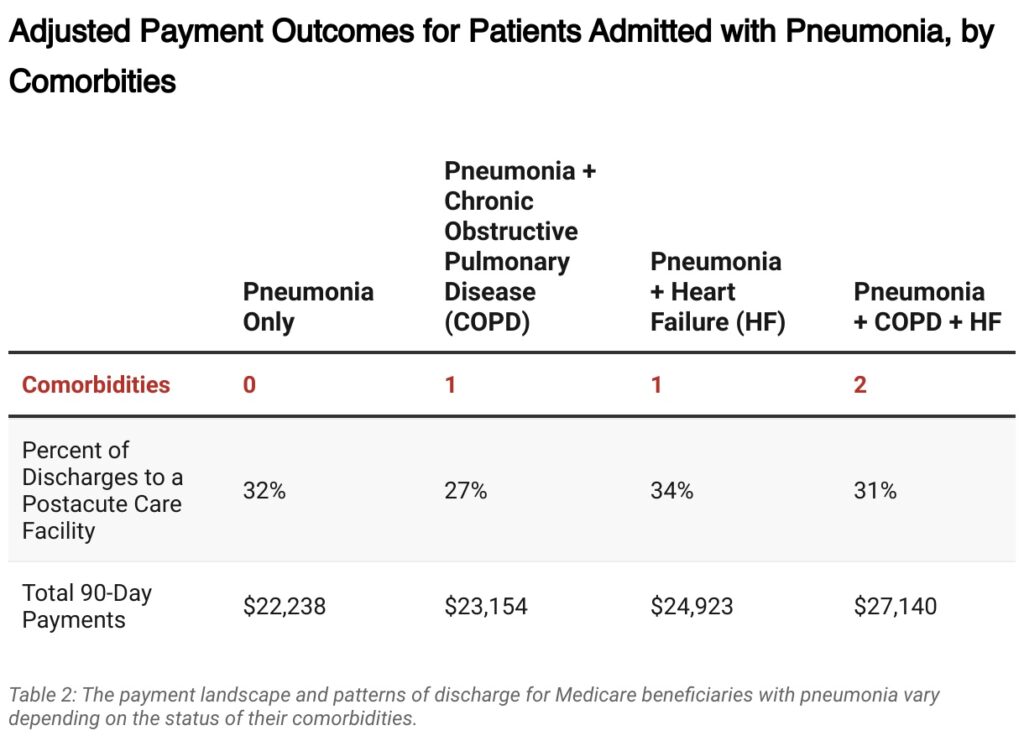
Common comorbidities of pneumonia, like chronic obstructive pulmonary disease (COPD) and heart failure, play a significant role in impacting treatment patterns and therefore the costs of care for patients with pneumonia. The investigators wanted to understand how comorbidities influenced the use of postacute care, such as the care provided by nursing facilities, since it accounts for a large part of the costs and/or savings in various bundled payments.
To explore the incidence of comorbidities for pneumonia and their association with costs and postacute care use, investigators examined hospital discharges of Medicare beneficiaries hospitalized for pneumonia, with and without these comorbidities, using Medicare claims data from 2010-2016.
Investigators found that, as hypothesized, patients with COPD and/or heart failure comorbidities had higher total payments in the 90 days after hospitalization. Unsurprisingly, the payments were highest among patients with more comorbidities compared to those with fewer.
Although, surprisingly, more comorbidities did not always translate into more time in institutional postacute care: Compared to patients with only pneumonia, patients with pneumonia and COPD—or with pneumonia, COPD, and heart failure—were less likely to be discharged to a facility, and those who were discharged to a facility spent fewer days there.
According to co-investigator Jessica T. Lee, “It actually makes clinical sense that patients who still qualify for hospital admission without the most common comorbidities might actually be sicker in ways that are hard to see in claims data, such as being unable to eat enough at home while they have pneumonia, factors that would influence their need for help after discharge. But that may mean that diagnoses that appear to be acute conditions, like infections, may require care that more reflects the patient status than the admission diagnosis, even when you adjust for comorbidities.”
These results highlight how a patient with pneumonia’s comorbid conditions can significantly influence their costs and course of care, offering valuable insight for planning value-based care interventions. Investigators advocate that in order to design the most effective alternative payment models for common conditions such as pneumonia and other conditions with high hospitalization rates, health care leaders and policymakers ought to consider comorbidities in addition to other patient characteristics.
The study, “Pneumonia is Not Just Pneumonia: Differences in Utilization and Costs with Common Comorbidities,” was published on October 10, 2023 in the Journal of Hospital Medicine. Authors include Jessica T. Lee, Amol S. Navathe, and Rachel M. Werner.


A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds
Research Brief: New Incentive Structures and Metrics May Improve Program Performance

Research Memo: Response to Request for Technical Assistance