
Toward a More Humane and Economically Viable Long-Term Care System
A Penn LDI Virtual Panel Looks Ahead at New Possibilities
Improving Care for Older Adults
Blog Post

Produced in conjunction with the Population Aging Research Center at the University of Pennsylvania.
For years, federal and state health agencies, including Medicare and Medicaid, have emphasized the need for older adults to have access to home and community-based services (HCBS) to support aging in place—living at home instead of at a long-term care facility. This is how more than two-thirds of adults prefer to spend late life. Yet as the U.S. population ages, the demand for HCBS exceeds the size of the workforce.
A new study led by former LDI Associate Fellow Katherine Miller and Senior Fellow Norma Coe, along with Katherine Ornstein from Johns Hopkins University, shows that for a growing number of older adults with disabilities in rural areas, family is their only source of help with daily activities such as eating, bathing, and shopping. The findings raise questions about how to support aging in place for rural residents.
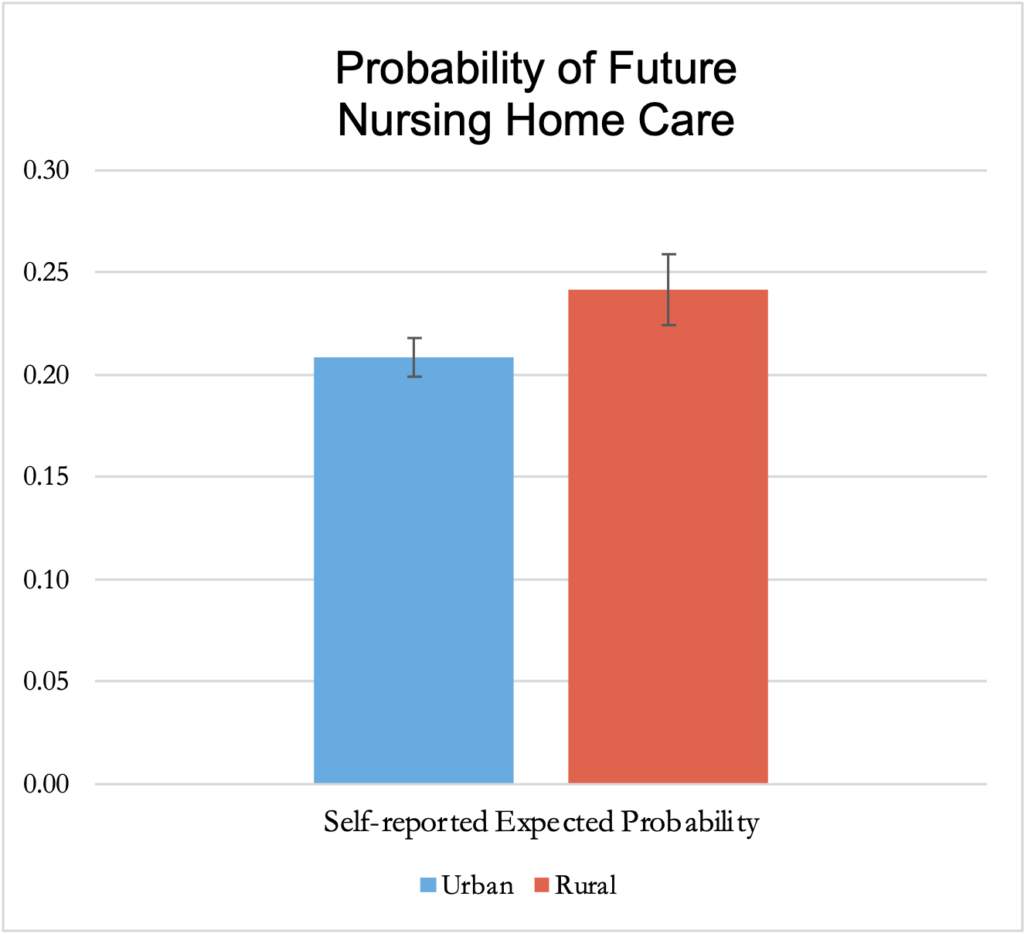
Miller and colleagues used data from a nationally representative survey of older U.S. adults to determine patterns of care for people who need help with at least two key tasks of daily living. In both rural and urban areas, care was most often from family members only, at 45% for rural residents and 40% for urbanites. Receiving care from only an unrelated, paid caregiver was the least common, at about 6% for rural and 8% for urban dwellers. About 23% overall reported getting no care at all. Rural residents were more likely than urban dwellers, by 2.5 percentage points, to receive any family care and they were more likely to receive care from family members only. They were also more likely than those in urban areas, by 4.4 percentage points, to receive any formal, paid home care, and to expect to use a nursing home in the next five years.
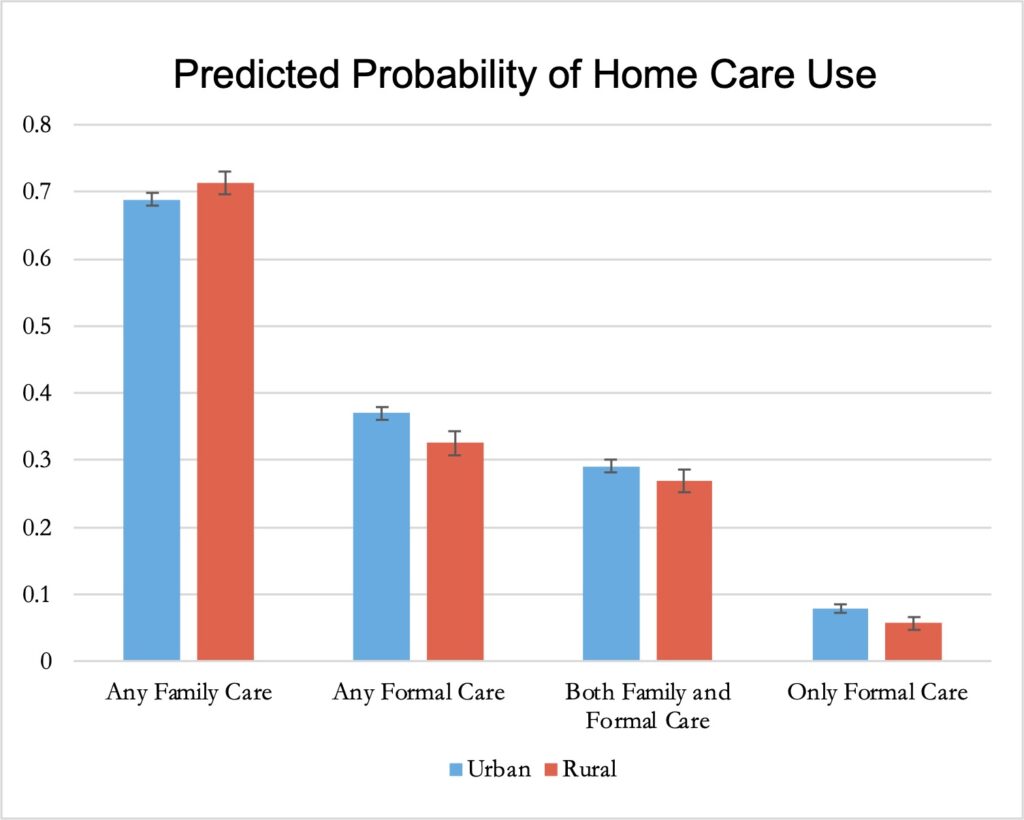
Miller’s research indicates rural residents may need more support than those in urban areas to ensure sufficient access to formal long-term services and support at home. They may also need greater support for their family caregivers. Miller and coauthors emphasize that giving and receiving family care has positive aspects. However, it is also a mental, physical, and financial strain that is known to be taxing to families.
Miller and colleagues urge policymakers to consider the impact on older rural residents and their families in balancing funding for nursing homes and HCBS. Their study demonstrates that national-level estimates about how older people receive care can mask significant differences in rural versus urban areas. They note that more in-depth research may find further differences within rural communities but existing studies show generally lower quality for rural compared to urban nursing homes.
The researchers plan to investigate whether the higher use of family caregivers in rural areas is due to preference or a lack of other options. “Our work is about ensuring access to formal care if it’s wanted and supporting family care if that’s preferred,” Miller said. “Our goal is supporting people in making the optimal choice for their care.”

The study, “Rural Disparities in Use of Family and Formal Caregiving for Older Adults with Disabilities,” was published on April 20, 2023 in the Journal of the American Geriatrics Society. Authors include Katherine E.M. Miller, Katherine A. Ornstein, and Norma B. Coe.


A Penn LDI Virtual Panel Looks Ahead at New Possibilities

Lessons from the Past, Imperatives for the Future

Technology Helps Older Adults Stay at Home—But May Delay Necessary Transitions to Higher Levels of Care

Her Transitional Care Model Shows How Nurse-Led Care Can Keep Older Adults Out of the Hospital and Change Care Worldwide

Direct-to-Consumer Alzheimer’s Tests Risk False Positives, Privacy Breaches, and Discrimination, LDI Fellow Warns, While Lacking Strong Accuracy and Much More

New Therapies Inspire Hope, Even as Access and Treatment Risks Continue to Challenge Patients and Providers