Acupuncture Could Fix America’s Chronic Pain Crisis–So Why Can’t Patients Get It?
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use
Blog Post


As wait times for appointments and administrative burden on U.S. physicians has grown, so has interest in concierge medicine. The model has been drawing patient and provider interest—and cautions from medical ethicists—for 25 years, but evidence on its effectiveness is just catching up.

A groundbreaking Journal of Health Economics study of primary care concierge medicine from LDI Senior Fellows Molly Candon and Guy David and Adam Leive at the Goldman School of Public Berkley at UC Berkley finds that the model draws healthier patients, increases health care costs, and does not impact mortality: The findings have access, cost, and equity implications for patients and the health care system at large.
In the concierge medicine primary care model, consumers receive increased access to their doctor (e.g., same-day appointments, longer visits) in exchange for an extra flat fee. There are several models but a common approach, and the model studied here, operates on top of an individual’s insurance coverage. The model is designed to provide “better” health care for the consumer, but does it actually improve the health—or extend the lives—of those who receive it? And what is the impact on health costs for those who enroll? If it provides more valuable time with a doctor, are those with higher health needs more likely to enroll?
The researchers found that concierge medicine enrollment corresponded with a sharp increase in total health spending for those that enrolled with no change in the patients’ mortality rates. Spending increased to 50% higher than before enrollment. They also found that patients’ health status did not affect their likelihood of selecting concierge medicine; instead, neighborhood income level had a stronger influence on the decision to join.
In addition to the difference in income level, the study showed that the patients who chose concierge medicine were slightly older, had fewer chronic conditions, and were more likely to be white. One year after a switch to concierge medicine, those patients who enrolled had health spending over 25% higher than a comparison group. Spending increases were driven by those who were in better health; both inpatient and outpatient spending rose. The study found little evidence that the risk of dying varied during the study period for those who enrolled in the concierge practice versus those who left the practice.
The researchers note that the study’s results are important to consider in light of access and equity goals. “If society prefers to increase health care access to people in worse health and those living in lower-income areas, then concierge medicine harms equity objectives,” the authors wrote, underscoring that the model does not appear to transfer more time and attention to patients in worse health.
Concierge medicine’s traditional appeal has been for the individual consumer and the primary care provider. The model has been built to increase access for those who are willing to pay and to reduce the burden on providers, by allowing them to serve a smaller group of patients. This study’s groundbreaking findings about health spending—a cost borne by insurers and payers of premiums—bring new information for patient advocates, public and private payers, and federal and state policymakers.
The study, “On Resource Allocation in Health Care: The Case of Concierge Medicine,” was published July 2023 in the Journal of Health Economics. Authors include Adam Leive, Guy David, and Molly Candon.

A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare
How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization

Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
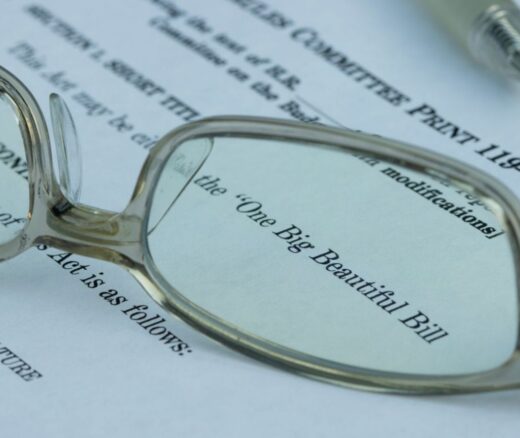
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector