Brief
Consumers’ Responses to Surprise Medical Bills in Elective Situations
The case of labor and delivery
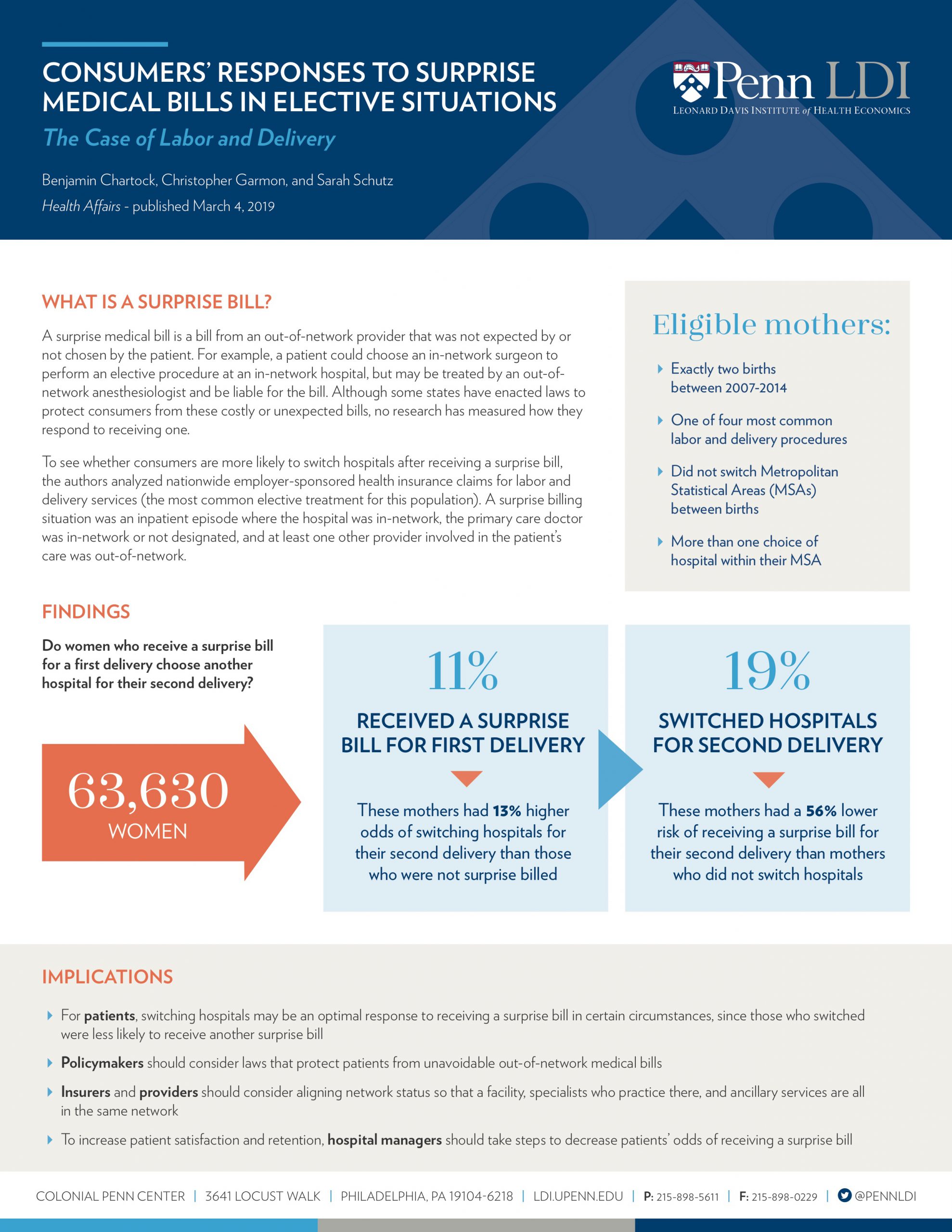
A surprise medical bill is a bill from an out-of-network provider that was not expected by or not chosen by the patient. Although some states have enacted laws to protect consumers from these costly or unexpected bills, no research has measured how they respond to receiving one. To see whether consumers are more likely to switch hospitals after receiving a surprise bill, Benjamin Chartock and Sarah Schutz, and their co-author Christopher Garmon, analyzed nationwide employer-sponsored health insurance claims for labor and delivery services (the most common elective treatment for this population). A surprise billing situation was an inpatient episode where the hospital was in-network, the primary care doctor was in-network or not designated, and at least one other provider involved in the patient’s care was out-of-network.
Click on the image below for findings published in Health Affairs: