
Hospital Mergers Don’t Make Care Better—They Just Make It Pricier, LDI Fellows Say
A New Review Finds Hospital Mergers Raise Prices Without Improving Care, and Urges Regulators to Stop Accepting Quality Claims to Justify Consolidations
Brief
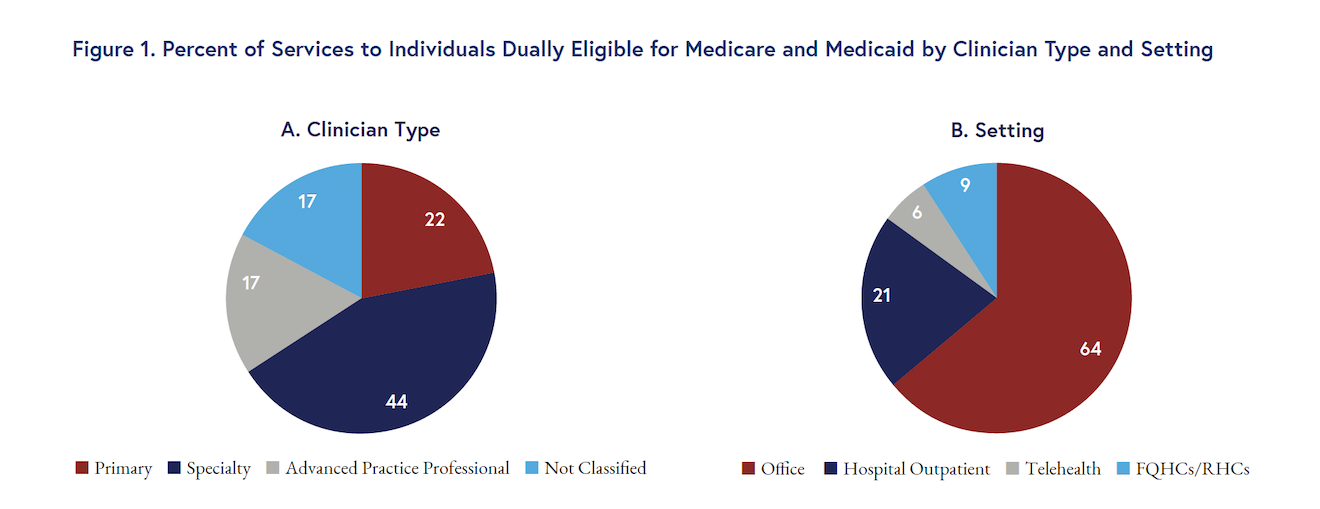
Outpatient care for people dually eligible for Medicare and Medicaid is heavily concentrated among a small number of clinicians and clinical practices. These practices are geographically dispersed, with substantial within-state variation and large areas where no practices routinely serve this population. Although Federally Qualified Health Centers (FQHCs) and Rural Health Clinics (RHCs) are traditionally considered the primary providers of outpatient safety net care, they deliver only 9% of these services to dually eligible individuals.
The more than 12 million U.S. adults with low incomes who are eligible for both Medicare and Medicaid tend to be sicker and face formidable challenges in getting care. These challenges are reflected in well-documented disparities in access and quality for this group. Policymakers cannot improve care for low-income individuals without a clear understanding of how they receive outpatient care—which is critical because most health care happens in clinics, doctor’s offices, and non-hospital settings.
A study led by former LDI Senior Fellow Joshua Liao, with LDI Senior Fellows Paula Chatterjee, Austin Kilaru, Amol Navathe, and colleagues, shows where individuals dually eligible for Medicare and Medicaid get outpatient care and who provides it. The work builds on this group’s study using 2013 data and complements efforts to help policymakers improve hospital care for low-income and other historically marginalized communities.
The researchers applied a method commonly used in economics to quantify inequality and demonstrated that outpatient care was unequally distributed among practices and heavily concentrated: 80% of outpatient services to dually eligible individuals came from only 0.3% of practices. About 14% of practices provided no outpatient care to this group.
The distribution of the practices delivering most of the care to dually eligible individuals varied across the U.S., with substantial within-state heterogeneity. In some areas, multiple, often adjacent counties provided few to no services. This variation was present across both rural and urban areas.
Compared to other Medicare beneficiaries, dually eligible individuals used fewer outpatient services overall and fewer specialty care services (Figure 1). Advanced practice professionals such as nurse practitioners and physician associates provided more than 17% of services to dually eligible individuals but under 13% of all services to their non-dually eligible counterparts.
The study supported the idea that FQHCs and RHCs are important parts of the outpatient safety net for dually eligible individuals. They received 9% of their outpatient care from these sites, which provided under 3% of these services to non-dually eligible individuals. However, dually eligible individuals received the majority of their outpatient care (91%) from clinical settings other than FQHCs and RHCs.
Outpatient care for low-income individuals dually eligible for Medicare and Medicare is unequally distributed, and this inequality has worsened over time. Comparing the new results to the researchers’ earlier work on clinicians who care for dually eligible individuals shows a greater concentration of services: In 2013, 35% of clinicians provided 80% of outpatient care to this group, compared to only 30% of clinicians providing this level of services in 2022. The descriptive findings also show a lower use of outpatient specialty care that suggests dually eligible individuals may face barriers to seeing medical specialists until they are sick enough to require hospitalization.
FQHCs and RHCs receive substantial safety net policy attention. However, the study found that other outpatient clinics often serve dually eligible individuals and should not be excluded from safety net policy considerations.
The researchers emphasized that to address challenges to outpatient care for dually eligible individuals, policymakers need consensus on what data and measures define the outpatient safety net. This clarity will inform evidence-based, transparent decisions that support practices disproportionately serving historically marginalized groups. Funding and policy reforms focused on the outpatient safety net could significantly improve access to and quality of care for low-income patients.
Future work from the researchers will examine the amount and variation in outpatient care among other groups, such as Medicaid-only beneficiaries. The team will also study the impact of the unequal distribution of care on patient outcomes and the relationship between outpatient and inpatient services in shaping these outcomes.
The researchers used 2022 data from the U.S. Census and the Centers for Medicare & Medicaid Services. The sample covered more than 106,545 practices and
815,827 clinicians, and nearly six million individuals, 967,820 of whom were dually eligible for Medicare and Medicaid, and 4.6 million who were not. This work was funded by Arnold Ventures (Grant 23-09141).
Source publication: Liao, J. M., Chatterjee, P., Zhao, Y., Carroll, I.J., Browne, D.S., Kilaru, A.S., Crowley, A.P., Pagnotti, D., Shirk, T., Cousins, D.S., Navathe, A.S. (2025). Ambulatory Care for Individuals Dually Eligible for Medicare and Medicaid. Health Affairs Scholar. doi.org/10.1093/haschl/qxaf148

A New Review Finds Hospital Mergers Raise Prices Without Improving Care, and Urges Regulators to Stop Accepting Quality Claims to Justify Consolidations

CMS’s Main Risk Adjustment Method Underestimates Rural Patients’ Health Risks, LDI Fellows Show, Potentially Reducing Access to Care in the Heartland

Experts at Penn LDI Panel Call for Rapid Training of Students and Faculty

A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

New Study From LDI and MD Anderson Finds That Black and Low-Income, Dually Eligible Medicare Patients Are Among the Most Neglected in Cancer Care

Her Transitional Care Model Shows How Nurse-Led Care Can Keep Older Adults Out of the Hospital and Change Care Worldwide