Acupuncture Could Fix America’s Chronic Pain Crisis–So Why Can’t Patients Get It?
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use
Could gene therapy break employer-sponsored health insurance at small companies? In Health Affairs Scholar, LDI Senior Fellows Jalpa Doshi, Atul Gupta, Mark Pauly, and Alexander Olssen say that despite the growth in gene therapy options and predictions about rising insurance costs, the expensive treatments do not threaten the U.S. health insurance system—as long as protections remain in place.
Gene therapies alter some of a patient’s genetic material to alleviate or eliminate disease. More than a dozen are currently available to treat rare conditions such as some cancers, hemophilia, and an inherited blindness. Gene therapies are technically challenging to develop and administer, and treatment can cost more than $1 million.
“There’s lots of excitement about these treatments and a number of them in the development pipeline,” Doshi said. “The concern is their huge upfront costs.” Insurers, employers, and some policy commenters worry that gene therapy could overwhelm a company providing employer-sponsored insurance.
Small firms under 200 workers are especially vulnerable, particularly if they are self-insured, meaning they do not offer coverage through a large insurer but provide their own health plan and bear the risks. Some health insurance analysts say the continued development of gene therapies could create unsustainable financial pressure on small, self-insured firms.
Doshi and coauthors have several reassuring messages for those worrying about the threat from gene therapy to employer-sponsored health insurance. They analyzed data from national surveys of employers to ask:
What is the size of the problem? How many employees work for companies susceptible to financial stress from a gene therapy claim?
How are these companies protected now—do they need new models to cover gene therapy?
The threat is overstated, the researchers’ analysis concluded, as long as certain conditions hold. Doshi and colleagues estimated that nationally, the number of employees at small firms that offer at least one self-insured plan is about 5 million—less than 5% of the civilian full-time workforce.
Even if a worker or other beneficiary at a small, self-insured firm received gene therapy, Doshi and colleagues estimate that stop-loss insurance purchased by employers would protect most against large claims. These external plans provide refunds for large payouts through either a single payment or a “level-funded” monthly rebate plan.
The researchers estimated that the proportion of the workforce currently in small, self-insured firms where employers lack stop-loss insurance, which would make financing a rare but high-cost gene therapy challenging, is tiny—under 2% of all full-time workers.
Plus, the likely number of workers in these firms who would need to get gene therapy is even smaller because it treats conditions that are exceedingly rare. For example, the authors estimated that fewer than 10 people a year at small, self-insured firms are expected to receive gene therapy for inherited blindness.
The study addresses additional concerns, such as the potential for an even steeper rise in stop-loss insurance premiums. Assuming gene therapies are cost-effective, providing value to employers and employees, the researchers argue that employers will provide coverage, in part to be competitive in recruiting and retaining workers. Even if some costs are passed to employees as higher premiums or decreased wages, the value of the coverage should mitigate this financial consequence.
The authors conclude that the current system of employer-paid, self-insurance supplemented by stop-loss coverage appears sustainable. As long as gene therapies are cost-effective, workers will value them and small, self-insured firms will cover them. Companies already cover rare, expensive procedures such as organ transplants.
For these reasons, alternative payment methods that spread costs over time or create special risk pools for people who might get gene therapy are not necessary—at least not yet, according to Doshi and colleagues. Designing and installing alternative payment models for the few workers in small, self-insured firms without stop-loss insurance who might need gene therapy is not worth the effort.
There is concern about a future “bonanza” of costly gene therapies for common conditions that will require employers to cover treatment for many people, Pauly said. However, despite the thousands of gene therapies in development, few actually make it to market. Those that do can be covered, if cost-effective, by small, self-insured firms with stop-loss protection.
Doshi and colleagues advise continued attention to gene therapies and the ability of the system, particularly stop-loss insurance, to be resilient to the introduction of these innovations. The sky is not falling with gene therapy, the authors say, but we need to keep looking up.
The article, “Is Employment Group Insurance Financing of Expensive Gene Therapies Threatened in the United States?,” was published on September 8, 2023 in Health Affairs Scholar as work funded by Spark Therapeutics. Authors include Jalpa A. Doshi, Morgan Eilers, Atul Gupta, Mark Pauly, and Alexander L. Olssen.

A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare
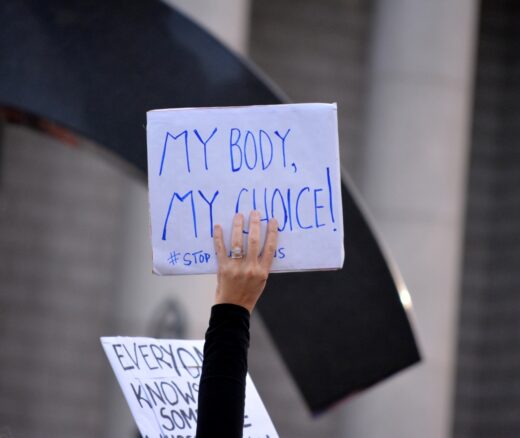
How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization

Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
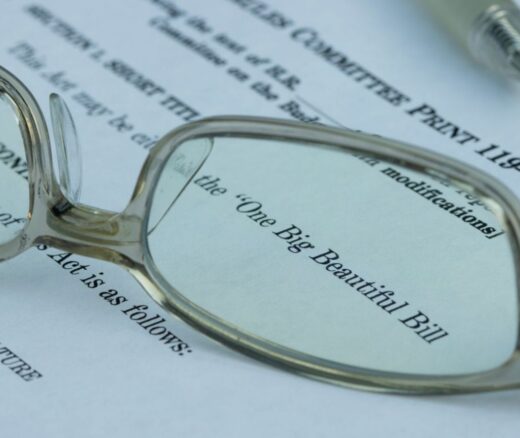
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector