
Medicare’s Hidden Fix for High Drug Costs
Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print
Blog Post
There is a shrinking number of publicly run hospitals in America. In the past quarter century, the share of all hospital beds at government-owned hospitals has declined by more than 40%. Many of these public hospitals were unprofitable but didn’t close — they were bought by a not-for-profit or for-profit health care system.
Privatizing hospitals in this way may keep their doors open, but how does it affect the provision of and access to care? LDI Senior Fellow Atul Gupta and colleagues studied the effects of nearly 260 privatizations of non-federal public hospitals from 2000-2018 on hospital finances and patient volume across payers.
Their study, recently released as a working paper by the National Bureau of Economic Research, revealed for the first time that while privatization substantially improves hospital profitability, enabling them to become financially sustainable even without government subsidy, patient volume decreases by 8.4%, with Medicaid patients experiencing the largest decline in care.
It’s possible that some of that care was unnecessary, but the results of the analysis indicate that privatized hospitals find ways to reduce the number of Medicaid patients they admit to minimize their exposure to unprofitable patients. While some patients appear to be absorbed by neighboring hospitals, the number of Medicaid patients being hospitalized declines at the market-level, which Gupta and colleagues interpret as a decline in access to care. As a result, Medicaid patients — now approximately 1 in 4 Americans — are “likely worse off due to privatization due to the disruption in their preferred provider and potentially because they may have to travel further or wait longer for treatment,” Gupta said.
Gupta listed several significant policy implications based on the study:
Whether Medicaid’s generally low payment rates are sufficient to ensure access to care is a growing concern: The study’s findings indicate that hospitals can’t recover their losses on Medicaid patients by overcharging privately insured patients, Gupta acknowledged. Other research has found that increased Medicaid reimbursement results in greater access to primary care. Taken together, these studies suggest that an increase in Medicaid reimbursement rates for hospital care might benefit both patients and health care markets.
Gupta and his colleagues are now focusing on learning more about how hospitals reduce the intake of unprofitable patients. To gain insight, they are studying some states with patient-level data, where a number of hospitals were privatized in a short period of time. They have obtained patient-level data on hospital discharges and plan to use it to explore the basis on which privatized hospitals reduce their intake of specific types of patients and which types of patients are hardest hit, such as patients with certain diseases or needing certain services. In addition, they plan to study whether quality of care changes following private ownership.
The study, “The Impact of Privatization: Evidence from the Hospital Sector,” was published on January 2023 as a Working Paper (No. 30824) by the National Bureau of Economic Research. Authors include Mark Duggan, Atul Gupta, Emilie Jackson, and Zachary S. Templeton.

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

Even With Lower Prices, Medicare, Medicaid, and Other Insurers Tighten Coverage for Drugs Like Mounjaro and Zepbound Using Prior Authorization and Other Tools

Pandemic-Era Medicare Flexibilities Have Proven Effective, Popular, and Safe

A 2024 Study Showing How Even Small Copays Reduce PrEP Use Fueled Media, Legal, and Advocacy Efforts As Courts Weighed a Case Threatening No-Cost Preventive Care for Millions
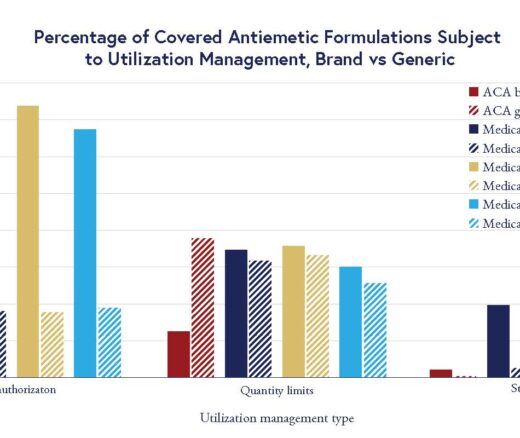
Chart of the Day: LDI Researchers Report Major Coverage Differences Across ACA and Medicaid Plans, Affecting Access to Drugs That Treat Chemo-Related Nausea

Insurers Avoid Counties With Small Populations and Poor Health but a New LDI Study Finds Limited Evidence of Anticompetitive Behavior