
Acupuncture Could Fix America’s Chronic Pain Crisis–So Why Can’t Patients Get It?
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use
Blog Post
Dual-Eligible Special Needs Plans (D-SNPs) are Medicare Advantage (MA) plans designed to serve people who qualify for both Medicare and Medicaid, and who often have chronic conditions and functional limitations.
Are these members more satisfied with integrated Special Needs Plans than with other Medicare Advantage options? They appear to be—at least on the important measure of disenrollment—according to a study by LDI Senior Fellow Eric T. Roberts and colleagues.
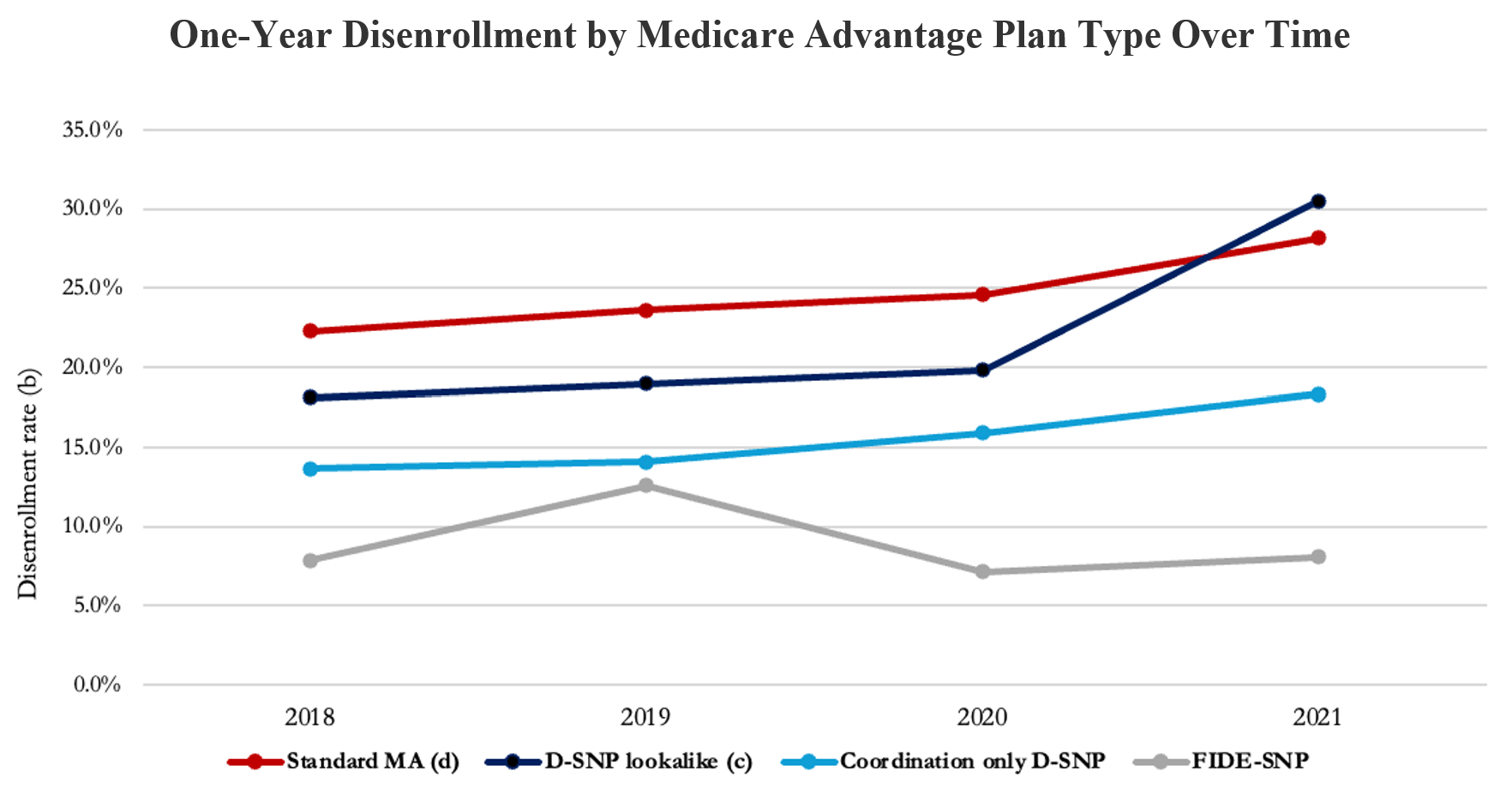
Their study looked at annual plan disenrollment rates—measured as the percentage of beneficiaries leaving plans—among 2.7 million dual-eligible individuals from 2018 through 2021. The researchers found substantial variation in disenrollment rates across Medicare Advantage plans that had different degrees of coordination with Medicaid.
Those enrolled in Fully Integrated Dual-Eligible Special Needs Plans (FIDE-SNPs) in 2021 had the lowest disenrollment rate—8.1% by 2022—among enrollees of all Medicare Advantage plan types. FIDE-SNPs integrate coverage of most Medicare- and Medicaid-funded services within a single health plan, which policymakers hope will lead to a more seamless experience for dual-eligible individuals.
Among those enrolled in coordination-only D-SNPs, which coordinate some care with Medicaid but do not directly manage Medicaid-funded services,18.3% left their plans.
Standard Medicare Advantage plans had the highest disenrollment rate at 30.5%, though Look-Alike D-SNPs also had a high rate at 28.2%. Neither of these plan types coordinates services or coverage with Medicaid.
About 29% of dual-eligible individuals are enrolled in D-SNPs. This population includes low-income individuals with complex health needs, chronic conditions, and functional limitations—some are older adults, while others are younger people with disabilities who qualify for Medicare and meet Medicaid eligibility due to limited financial resources.
A variety of Special Needs Plans exist, and among them, FIDE-SNPs are considered the most integrated. However, little is known about how well plans meet the needs of the people they are intended to serve. One way to measure how satisfied people are with their health care coverage is to look at disenrollment rates because leaving a plan may indicate dissatisfaction.
Lower disenrollment rates among FIDE-SNPs compared to Medicare Advantage plans with less integration align with expert calls for more access to integrated care for dual-eligible individuals. These findings could inform efforts to create health care coverage that works best for low-income individuals with complex care needs.
The study, “Enrollment in Dual-Eligible Special Needs Plans and Disenrollment Rates” was published July 3, 2025, in JAMA Health Forum. Authors include David J. Meyers, Eliza Macneal, Kendra Offiaeli, and Eric T. Roberts.


A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare

How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization

Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies

They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector