
Penn LDI CICADA Initiative Names Researchers for 2025-2026 Cohort
Eighth Year of Program That Recruits, Mentors and Develops Junior Faculty for Health Services Research
Blog Post
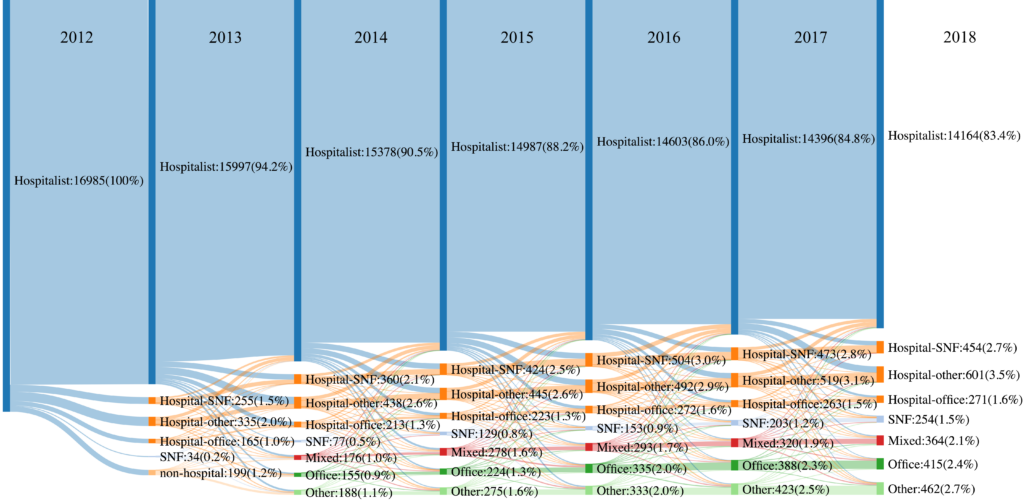
It’s been more than 15 years since Wachter & Goldman named the burgeoning specialty of inpatient medicine “hospitalists,” and since then, hospitalists have effectively taken over care of hospitalized patients in the U.S. In a JAMA Health Forum study (and illustrated vividly in the chart above), my colleagues and I delve into the career trajectory and stability of these hospitalists.
We followed a cohort of 16,985 hospitalists in 2012 for seven years, and found that 1 in 4 shifted practice outside of the hospital at least temporarily (1 year or more). The chart shows movement of hospitalists to other settings over time, with some returning back to practice exclusively in the hospital.
Given the predominance of hospitalists in inpatient care, these findings have important implications for hospitals, who face the significant costs of hospitalist turnover, and for the quality of patient care. Most recently, the pandemic placed unprecedented demands on hospital-based clinicians, potentially creating even more career instability.
The study, Practice Trends and Characteristics of US Hospitalists from 2012 to 2018, was published in JAMA Health Forum on November 5, 2021. Authors include Kira L. Ryskina, Kaitlyn Shultz, Mark Aaron Unruh, and Hye-Young Jung.

Eighth Year of Program That Recruits, Mentors and Develops Junior Faculty for Health Services Research

Comment: Delivered to the U.S. Department of Labor
Less Than 1% of Clinical Practices Provide 80% of Outpatient Services for Dually Eligible Individuals

From Anxiety and Loneliness to Obesity and Gun Deaths, a Sweeping New Study Uncovers a Devastating Decline in the Health and Well-Being of U.S. Children

Chart of the Day: National Study Shows White Patients More Likely Than Black Patients to Get CT and/or Ultrasounds for Abdominal Pain in the Emergency Department

Hospitals and Physician Groups Can Also Benefit From Those Payments, as Medicare Launches a New Model for Episodic Care