
Experts: Medicaid Cuts Could Prove Fatal for Thousands
Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds
Blog Post
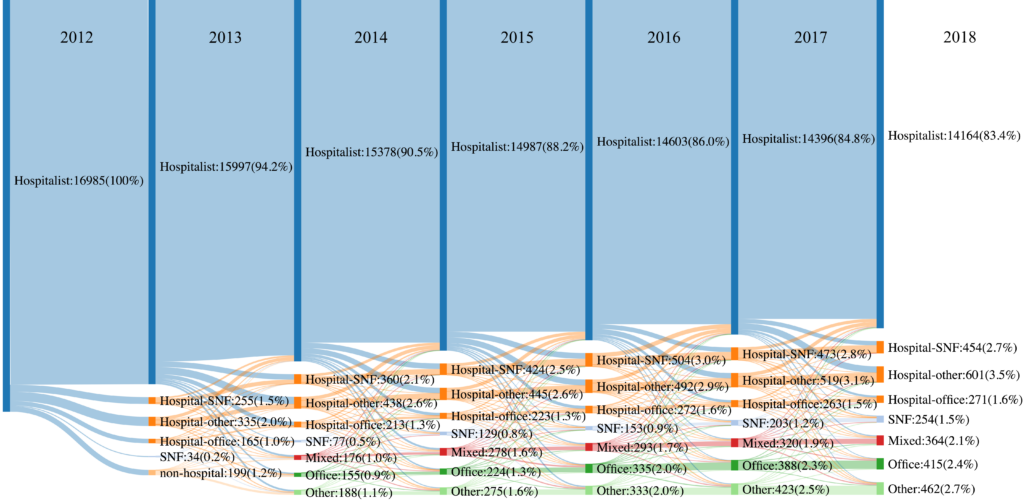
It’s been more than 15 years since Wachter & Goldman named the burgeoning specialty of inpatient medicine “hospitalists,” and since then, hospitalists have effectively taken over care of hospitalized patients in the U.S. In a JAMA Health Forum study (and illustrated vividly in the chart above), my colleagues and I delve into the career trajectory and stability of these hospitalists.
We followed a cohort of 16,985 hospitalists in 2012 for seven years, and found that 1 in 4 shifted practice outside of the hospital at least temporarily (1 year or more). The chart shows movement of hospitalists to other settings over time, with some returning back to practice exclusively in the hospital.
Given the predominance of hospitalists in inpatient care, these findings have important implications for hospitals, who face the significant costs of hospitalist turnover, and for the quality of patient care. Most recently, the pandemic placed unprecedented demands on hospital-based clinicians, potentially creating even more career instability.
The study, Practice Trends and Characteristics of US Hospitalists from 2012 to 2018, was published in JAMA Health Forum on November 5, 2021. Authors include Kira L. Ryskina, Kaitlyn Shultz, Mark Aaron Unruh, and Hye-Young Jung.

Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds

Cited for “Breaking New Ground” in the Field of Hospital Operations

Men are Stepping Up at Home, but Caregiving Still Falls On Women and People of Color LDI Fellow Says

More Flexible Methadone Take-Home Policy Improved Patient Autonomy

Penn LDI Seminar Details How Administrative Barriers, Subsidy Rollbacks, and Work Requirements Will Block Life-Saving Care

His data-driven initiatives risk violating consent, spreading stigma, and reviving vaccine misinformation, LDI Fellow writes.