Acupuncture Could Fix America’s Chronic Pain Crisis–So Why Can’t Patients Get It?
A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use
Blog Post

If you think Medicare beneficiaries don’t have to worry about paying for health care, think again. Medicare recipients spend more on health care than people with other types of insurance. One-quarter struggle to pay their premiums. For more than one-third, the extra costs of a hospital visit create persistent stress about their finances or financial precarity, causing some to delay needed care. Policymakers and insurers want to address the issue but questions remain about the best way to identify those who need help and how much help to give them.
In an Annals of Internal Medicine study, Penn LDI Senior Fellows Paula Chatterjee and Eric Roberts and their colleagues sought to understand the scope of financial precarity among Medicare recipients when they need to cover the out-of-pocket cost of a hospital visit.
They gathered data from a representative sample of Medicare-enrolled respondents with income between 100% and 400% of the federal poverty level selected from the 2018 Health and Retirement Study (HRS). Then they estimated the percentage of people who would be unable to pay the Part A Medicare deductible ($1,600) for a hospital stay.
The potential for financial hardship from hospitalization existed at all asset levels and was greater among beneficiaries who were Black and Hispanic, chronically ill, and with lower educational attainment.
The amount of financial stress changed depending on how the researchers assessed peoples’ financial resources (e.g., balances in checking and savings accounts vs. all liquid assets), if they considered the need to reserve funds for future living costs, and whether members had supplemental insurance.
In all situations, the proportion of beneficiaries facing financial precarity from the Part A hospital deductible exceeded 30%. Specifically,
The findings show that older adults at the same modest income level may not have a similar ability to pay for hospitalization. Additionally, there are racial and socioeconomic disparities in the risk of financial hardship due to such expenses.
Based on their findings, Chatterjee and colleagues suggest policymakers consider the following ways to protect older adults from financial hardship due to hospitalizations:
Expanding financial protections to include a broader range of beneficiaries—especially those with moderate incomes and limited savings—would help ensure that U.S. older adults are not forced into poverty because they go to the hospital for needed health care.
The study, “Risk for Financial Precarity from Hospitalization: Implications for Targeting Financial Assistance in Medicare” was published on October 29, 2024 in Annals of Internal Medicine. Authors include Paula Chatterjee, Eliza Macneal, Syama Patel, and Eric T. Roberts.

A Proven, Low-Risk Treatment Is Backed by Major Studies and Patient Demand, Yet Medicare and Insurers Still Make It Hard To Use

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities
Research Brief: Shorter Stays in Skilled Nursing Facilities and Less Home Health Didn’t Lead to Worse Outcomes, Pointing to Opportunities for Traditional Medicare
How Threatened Reproductive Rights Pushed More Pennsylvanians Toward Sterilization

Abortion Restrictions Can Backfire, Pushing Families to End Pregnancies
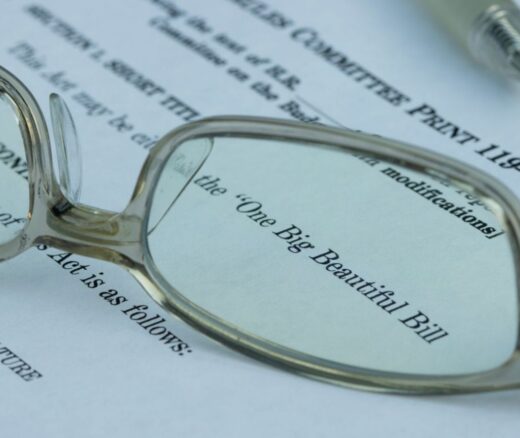
They Reduce Coverage, Not Costs, History Shows. Smarter Incentives Would Encourage the Private Sector