Blog Post
Physician Perspectives Towards Medicare’s New Payment Program
A survey of physicians in year 1 of MIPS
In a study in Health Affairs, LDI Senior Fellow Joshua Liao and colleagues report on what physicians think about Medicare’s new payment program, the Merit-based Incentive Payment System (MIPS). The authors found that in the first year, few physicians reported being familiar with the new payment policy designed to shift compensation from volume to value, and when informed, nearly 60 percent believed it would reduce or have no effect on the value of care.
Liao and colleagues, including LDI Senior Fellows Judy Shea and Amol Navathe, surveyed a national sample of 1,431 internal medicine physicians, slightly over half of whom responded. First the authors asked the physicians about four broad areas that could increase the value of care: reporting and performing well on clinical quality measures, initiating or participating in practice improvement activities, controlling patients’ resource use, and implementing and using electronic health records (EHRs). Respondents were not informed that these areas reflect the four domains that determine a physician’s score and payment under MIPS.
Most respondents (54-71 percent) believed that physician efforts in each area could “somewhat or significantly improve” the value of care, and more than half said that they were willing to change their behavior in each area for the sake of value. However, only 36-45 percent believed physicians have some control over these areas, and 35-41 percent believed that some compensation should be tied to these activities.
MIPS began on January 1, 2017 under the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). MACRA repealed the Medicare Part B Sustainable Growth Rate formula and replaced it with value-based payment policies. Non-exempted Part B physicians who do not participate in Advanced Alternative Payments Models will be paid under MIPS, the nation’s largest physician pay-for-performance program to date.
The survey findings, gathered from March-May 2017, signal the need for continued physician outreach and education about MACRA and how it changes the way physicians are paid. Once informed of the MIPS domains in the survey, 38 percent of respondents believed MIPS would improve the value of care, 21 percent believed it would reduce the value of care, and 41 percent thought it would have no impact. Respondents who reported personal compensation being tied to cost or quality incentives were more likely to believe MIPS would improve value than those without these incentives.
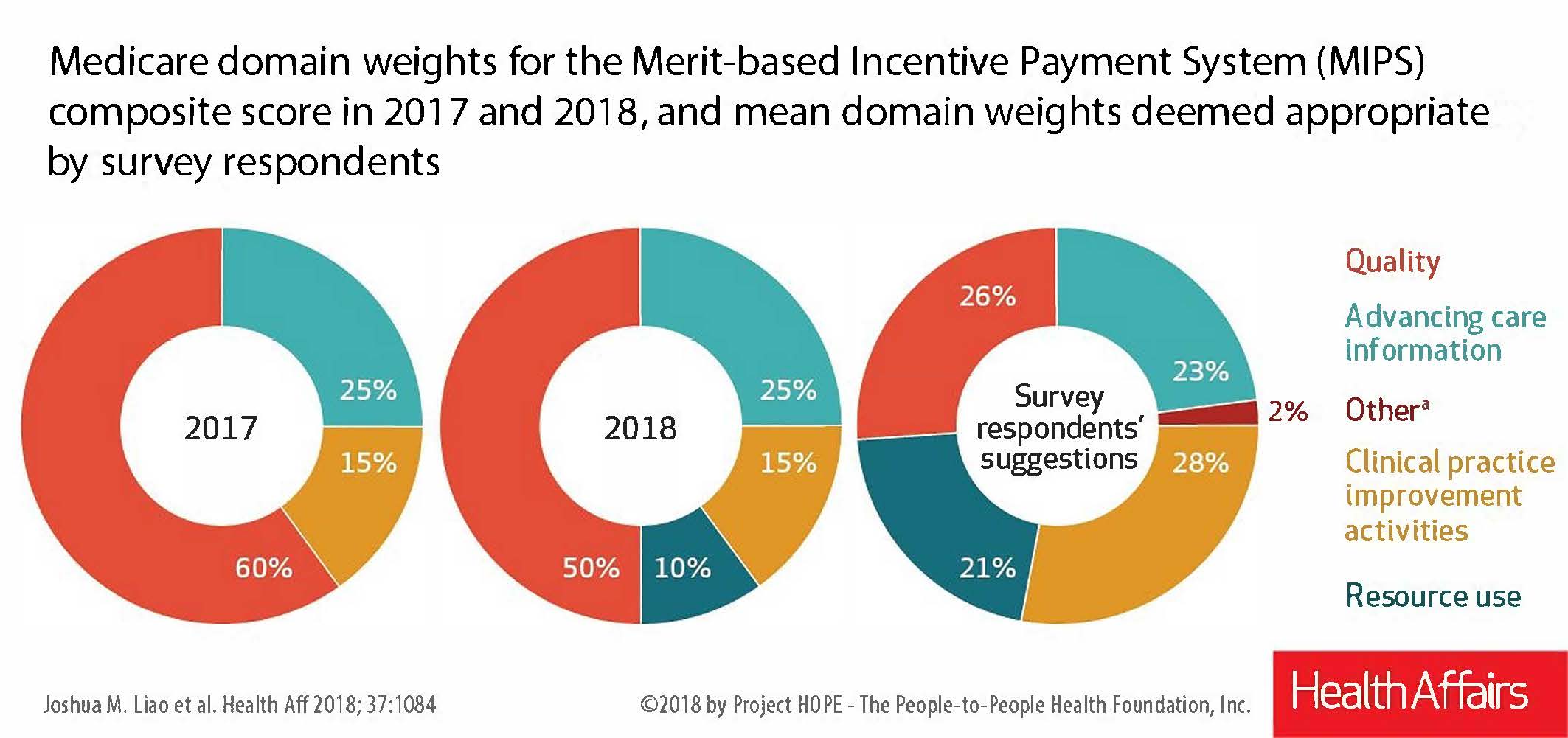
Since MIPS weights physician performance in four domains to generate a composite score that determines Part B compensation, respondents were asked to provide what they believed were appropriate weights for each domain. On average, respondents assigned percentages to all but one domain (“advancing care information”) that were much higher or lower than those actually assigned to each domain in 2017 and 2018. Some respondents also suggested other areas they believe should be included in a physician’s MIPS score (see figure below).
Most significantly, more than half of respondents believed that MIPS’s pay-for-performance structure could have negative, unintended consequences for physician behavior and patients, such as causing physicians to focus on MIPS-measured care to the detriment of unmeasured care; encouraging physicians to avoid sicker or more complex patients; and incentivizing physicians to change clinical documentation to improve their performance on quality measures. To guard against these unintended consequences and “gaming of the system,” the authors suggest that policymakers review physicians’ coding practices and quality metrics submitted for 2018 and beyond.
The Centers for Medicare and Medicaid Services (CMS) recently proposed a number of changes to MIPS for 2019. CMS is now collecting public comments on the proposed changes, which present an opportunity to improve MIPS by incorporating physician perspectives into the program. Overall, the authors note that more closely aligning MIPS policies and physicians’ perspectives could maximize MACRA’s impact on physician performance and payment.