
Medicaid Long-Term Services and Supports Data
Issue Brief: Understanding Gaps and Opportunities to Advance Research and Policy
Improving Care for Older Adults
Blog Post
COVID-19 has cast a light on the need for high-quality long-term care, and experts are anticipating heightened demand for home health care due to the high rates of COVID-19 infections and deaths in nursing homes. Home health care provides skilled nursing services and other therapies in patients’ homes and therefore relies heavily on nurses. As of 2018, the home health care industry employed more than 250,000 registered and licensed practical nurses nationwide.
While we know that high levels of turnover among nurses can compromise the quality of patient care in hospital and nursing home settings, we don’t have much evidence on nursing turnover and its determinants in home health. Home health care is distinctive in how providers operate—rather than team-based set-ups, nurses work independently, traveling from house to house. A potential driver of turnover, unique to home health care, is schedule volatility, or the variation in daily schedules. Studies suggest that scheduling concerns are a key contributor to nursing turnover, but the lack of administrative data make it difficult to verify in real world settings.
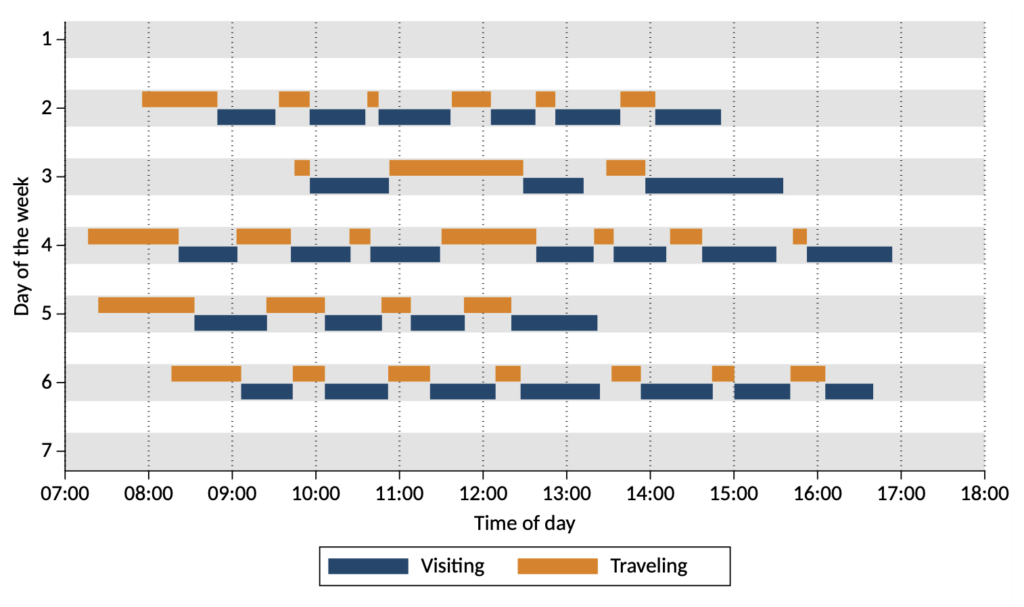
Until now. In our new paper in Medical Care Research and Review, we used human resources and visit-level data from one of the largest home health organizations in the U.S. and tracked the variability in daily visits between 2016 and 2019 for more than 1,000 full-time and part-time registered and licensed practical nurses. As illustrated in Figure 1, we found large fluctuations in each nurse’s day-to-day activities, including number of visits, visit length, and travel times between visits.
We found a strong relationship between schedule volatility (as measured by the variability in the daily number of visits over the past month), and a full-time nurse’s likelihood to quit. Nurses with extreme values of schedule volatility were more greatly affected; for example, full-time registered nurses with the least volatile schedules (in the 5th percentile) were 40% less likely to quit than average, while full-time registered nurses with the most volatile schedules (in the 95th percentile) were 50% more likely to quit.
Notably, the relationship between schedule volatility and turnover disappeared for part-time nurses, suggesting that their preferences for scheduling are different from those in full-time positions. It also demonstrates why any intervention that targets scheduling volatility cannot be one-size-fits-all. Instead, interventions should be tailored to account for differences in nurses’ preferences for variability in scheduling.
While our data predate COVID-19, the pandemic adds new context as workers demand more flexible scheduling. In the last year, high rates of burnout have resulted in high rates of turnover among nurses. Our research highlights a straightforward approach to flagging nurses at increased risk of quitting stemming from scheduling practices, and we are now working with our industry partners to pilot-test interventions to identify nurses at risk of quitting and to address scheduling issues to improve retention. Finding new ways to mitigate turnover among home health nurses could increase the quality of care delivered to millions of Americans.

The study team includes Alon Bergman, a postdoctoral fellow at LDI, Hummy Song, an Assistant Professor of Operations, Information and Decisions at the Wharton School, Guy David, the Department Chair of Health Care Management at the Wharton School, Joanne Spetz, the Director of the Philip R. Lee Institute for Health Policy Studies, Associate Director for Research, Healthforce Center, and the Brenda and Jeffrey L. Kang Presidential Chair in Healthcare Finance at University of California, San Francisco, and Molly Candon, an Assistant Professor of Psychiatry and Health Care Management. This research was supported in part by the Population Aging Research Center at Penn, the National Institute on Aging, and the Health Resources and Services Administration.


Issue Brief: Understanding Gaps and Opportunities to Advance Research and Policy

A Penn LDI Virtual Panel Looks Ahead at New Possibilities

Lessons from the Past, Imperatives for the Future

Technology Helps Older Adults Stay at Home—But May Delay Necessary Transitions to Higher Levels of Care

Her Transitional Care Model Shows How Nurse-Led Care Can Keep Older Adults Out of the Hospital and Change Care Worldwide

Direct-to-Consumer Alzheimer’s Tests Risk False Positives, Privacy Breaches, and Discrimination, LDI Fellow Warns, While Lacking Strong Accuracy and Much More