News
An Innovative-Thinking Retreat for Mental Health Care Innovation Researchers
Penn ALACRITY Event Pulls Scientists Away From Their Comfort Zone and Traditional Assumptions

Launched in 2017 and funded by a P50 grant, Penn’s “Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness” (ALACRITY) research project is the first of its kind. It’s a collaborative effort between the Center for Mental Health (CMH) and the Center for Health Incentives and Behavioral Economics (CHIBE) aimed at studying how behavioral economics and implementation science can be combined to improve community mental health care services.
“One of the truly exciting and rewarding aspects of this retreat is that it highlights the value of academic-community partnerships such as ours. We work with our city partners to identify challenges they face that are of great public health concern. Then, through the resources ALACRITY affords us, we gather content and methods experts to address these challenges,” said David Mandell, ScD (above, left), Director of Penn’s Center for Mental Health and Senior Fellow at the Leonard Davis Institute of Health Economics (LDI).
“For me, the most noteworthy part of these retreats is the magic and lightbulb moments that happen when we engage in multidisciplinary and divergent thinking that generates new insights,” said Rinad Beidas, PhD (above, right), Director of the Penn Implementation Science Center at the Leonard Davis Institute and LDI Senior Fellow.
Mandell and Beidas, along with Penn Medicine’s Kevin Volpp, are the three principal investigators on the ALACRITY grant.
Roy Rosin, MBA (above, right), Chief Innovation Officer of Penn Medicine since 2012, offered fresh insights about innovative thinking and problem solving, observing that researchers in search of a solution often define the wrong problem. He told the fascinating story of a young researcher studying severe anemia in Cambodian fishing villages. Clinicians there viewed the primary problem as their patients’ refusal to change their diets or take iron supplements that caused unpleasant side effects. The young researcher realized the actual problem was that the villagers needed to ingest more iron. He also knew that cast iron pots leached iron into the food they cooked, and that Cambodian culture revered the giant Mekong Barb fish as a symbol of luck, health and national pride. The researcher created a tiny metal version of that beloved creature, called it “the Lucky Iron Fish,” and convinced villagers to drop one in their woks of soup and stews. The unusual intervention introduced more iron into the daily diet and ultimately reduced anemia incidence by 50%.
In the retreat audience was Philadelphia Commissioner of Behavioral Health and Intellectual disAbility Services (DBHIDS) David Jones (above, left), whose agency provides behavioral health coverage for the City’s 700,000 Medicaid recipients through 11 community mental health centers and 35 other specialized facilities. Above, right, the Medical Director of DBHIDS’ Community Behavioral Health (CBH), Geoffrey Neimark, MD, presented on the status of efforts to address the opioid epidemic. He pulled no punches about one of the greatest obstacles to that endeavor: the failure of many providers to use medication-assisted treatment (MAT). “There’s a fairly large disconnect,” he said. “MAT is the gold standard, but despite enormous amounts of robust evidence about its efficacy, there is a continuing philosophical dispute around its use in the treatment of opioid use disorder.” Neimark is also a Clinical Assistant Professor of Psychiatry at Penn’s Perelman School of Medicine.
Also addressing the issue of medication-assisted treatment (MAT) for opioid use disorder was Rebecca Stewart, PhD (above, left), a faculty member at the Penn Center for Mental Health, LDI Associate Fellow, and researcher focused on the use of evidence-based practices in the substance abuse treatment field. Her recent city-wide survey of treatment providers contracted by the City of Philadelphia found that about 64% percent of them use some form of medication-assisted treatment (MAT). That dramatically exceeds the national average of only 36% of treatment facilities that use the evidence-based MAT practices. Stewart noted that DBHIBS has issued new payment rules effective January 1 of 2020 mandating the use of MAT. “Studies in France and Baltimore show that when you add buprenorphine and methadone to treatment, deaths go down, and when you take those away, deaths go up,” Stewart said. “The new Philadelphia MAT mandate is a really clear indication that City leadership is strongly signaling its priorities.”
In keeping with the retreat’s focus on new ways to think about innovative health care delivery solutions, Innovation Design Strategist Michael Begley, MA (above, left), hosted a card game created by the Penn Medicine Center for Health Care Innovation. Called “Accelerators in Health Care,” the game is an intense mental exercise that moves players out their comfort zone and away from their normal assumptions. After the audience was split up into teams, each received a health care challenge card and three “booster” cards (above, right) that suggested strategies used in other industries to address logistical, management and delivery problems. Viewing their assigned challenge through those filters, team members came up with solution ideas and pitched them to their table’s judge, who selected a winner. In between, there were as many quizzical looks as their were spirited debates and discussions across the tables.
At the end of the “Accelerators in Health” Care session, team leaders reported on their challenges and the new sorts of solutions they came up with. Above, left, explaining her team’s work is Suet Lim, PhD, Director of Research at Philadelphia DBHIBS. Behind her to the left is Penn Social Policy & Practice Associate Professor and LDI Senior Fellow Steven Marcus, PhD. Above, right, Brienne Jennings, MA, a former operational specialist for CBH’s Evidence Based Practice and Implementation Center, recaps her team’s bout of innovative thinking.
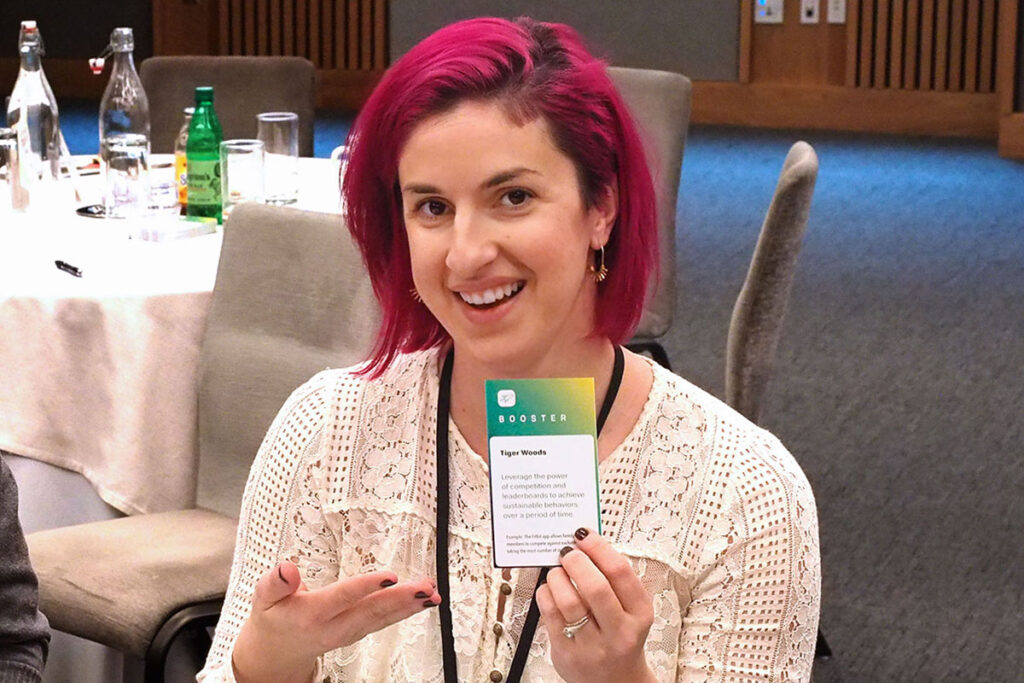
CBH Evidence-Based Practice Implementation Specialist Amber Lee Venti, MA, BCDMT, LPC (above, left), displays her “Accelerators in Health Care” suggestion to envision a solution based on insights from Tiger Woods. It reads, “Leverage the power of competition and leaderboards to achieve sustainable behaviors over a period of time.” Above, right, Penn Medicine Center for Health Care Innovation Operations Director and LDI Senior Fellow Shivan Mehta, MD, MBA, makes a point about a potential solution strategy.
Mia Everett, MD (above, left), Medical Director for Children’s Services at CBH, and her two clinical managers, Lauren DellaCava, MSW, Clinical Director, Children’s Services, and Kristen Vescio (above, right), Clinical Coordinator for Children Services, discussed one of their agency’s major challenges: Philadelphia’s Psychiatric Residential Treatment Facilities (PRTFs). These are 24/7 live-in facilities for the treatment of teenagers with significant mental illnesses or emotional disturbances. But the PRTF treatment approach has never been supported by evidence and, since 2006, there have been concerted efforts to reduce its use. In 2006 there were 2,759 Philadelphia PRTF patients. By 2017, that number had been reduced to 565 patients, each of whom stays in the PRTF system an average of about 300 days.
Among the reasons cited for the difficulty of moving away from PRTF further are family engagement, the clinical complexity of the PRTF patients, the availability of after-care resources, the particular challenges of teenagers with neuro-developmental disorders, and the involvement of the courts. “There is a lot of evidence for other evidence-based treatments that take place in the community (like those) we offer through family-based services,” the CBH presenters said.
Other enthusiastic participants in the audience included (above, left), Perrin Fugo, BA, Clinical Research Coordinator at the Penn Center for Mental Health and (above, right) David Oslin, MD, Professor of Psychiatry at Philadelphia’s Crescenz VA Medical Center.