
Over 500 U.S. Hospitals Have Stopped Delivering Babies Since 2010
A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike
Blog Post
Health care providers in the United States are burnt out. The ongoing COVID-19 pandemic is a major driver of current burnout, but the roots of the crisis run deep, embedded in decades-old reimbursement policies that impose high administrative burdens on providers. In an attempt to mitigate this burden, the American Medical Association (AMA) and Centers for Medicare and Medicaid Services (CMS) revised the regulations governing how providers use Evaluation and Management (E/M) billing codes. Our new Annals of Internal Medicine study shows that this major overhaul—effective January 1, 2021— did change how providers bill, but hasn’t yet materialized into reduced provider burden.
The 2021 E/M changes aimed to both simplify billing logic and reduce documentation burden. The clinical logic to determine the right “level of service” for a visit can be ambiguous at times, leading to difficulty in applying the correct (i.e. highest level) E/M codes. To remove this ambiguity in E/M billing, the clinical logic for matching visits to levels of service was streamlined, reducing this administrative burden and making it easier to bill at higher levels.
To reduce documentation burden, the AMA and CMS relaxed requirements dictating what information had to be included in clinical notes. These documentation requirements have been blamed for the extraordinarily long clinical notes found in U.S. electronic health records (EHRs) and the extensive time U.S. providers spend in the E.H.R., a key driver of burnout.
In the wake of these changes, our study aimed to answer two main questions. First, did providers change their E/M billing in response to simplified billing logic? And second, did they change their documentation to remove the content that is no longer required and thus reduce overall note length? We used weekly measures of billing and system use derived from the EHR activity of more than 300,000 U.S. outpatient providers using Epic, the leading EHR vendor.
We found an immediate shift in E/M billing following the new guideline, with providers reducing Level 3 billing and sharply increasing the share of E/M visits billed to Levels 4 and 5, the most expensive and highest-complexity visits. Unfortunately, notes stayed stubbornly long, as did the average time providers spent in the EHR writing notes.
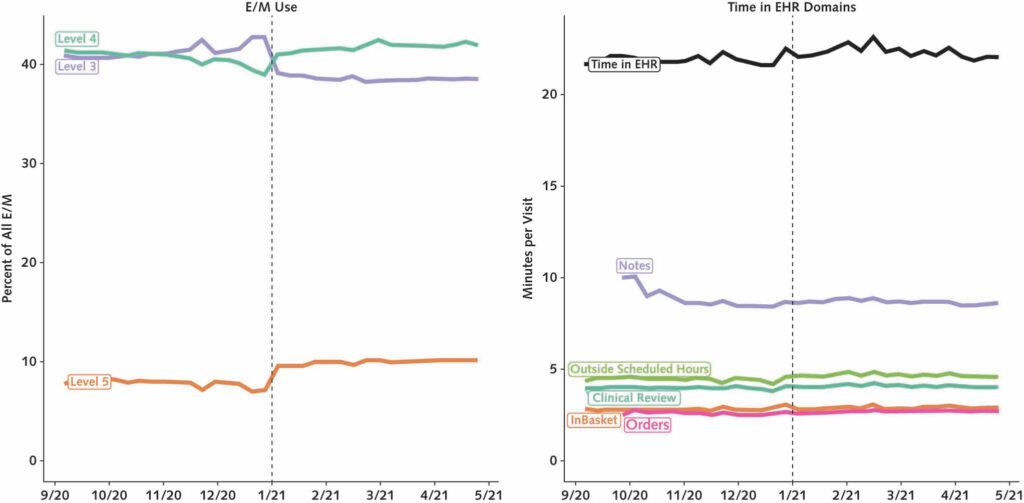
What surprised us was not just the immediacy and subsequent stability of the E/M billing changes, but how these changes varied widely across specialties. Primary care providers roughly mirrored the overall average trends, but some specialties, like dermatology, made more dramatic changes. Dermatologists, on average, shifted their Level 4 E/M billing from 22% of all E/M visits to 34% after the new policy, a more than 50% increase. The second-largest change was among endocrinologists, who shifted Level 5 billing from 15% to 19% of all E/M visits.
The policy implications of these findings are two-fold. First, the shifts we’ve identified will represent a substantial increase in spending on E/M services, which already comprise a significant amount of outpatient U.S. health care spending. In 2019, Medicare alone spent $16.2 billion on the 10 E/M codes we analyze in our study. Combine that with the fact that these billing changes—and our study—apply to all payers (not just Medicare) and included increases in E/M reimbursement rates, and we are looking at an enormous net increase in E/M spending in 2021, especially compared to the “down” pandemic year of 2020.
This spending increase isn’t necessarily problematic, but the second policy implication has to do with the distribution of these spending increases. Our back-of-the-envelope math suggests that this level-shifting alone will increase overall E/M payments to dermatologists by 12%, compared to just three percent for primary care. This inequity may exacerbate, rather than ameliorate, existing payment disparities between primary care and specialties.
The lack of any impact on documentation or time in the EHR is discouraging, but it may simply take more time for providers to modify their existing note-writing styles, which have developed over years of clinical practice. For researchers like me, interested in how we can optimize the use of technology to support health care delivery, our findings also raise the question of how to best measure and reduce provider EHR burden.
The study, Early Changes in Billing and Notes After Evaluation and Management Guideline Change, was published February 22, 2022, in the Annals of Internal Medicine by Nate C. Apathy, Allison J. Hare, Sarah Fendrich, Dori A. Cross.


A Crisis in Maternal Care is Unfolding—and it’s Hitting Rural and Urban Communities Alike

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds
Research Brief: New Incentive Structures and Metrics May Improve Program Performance

Research Memo: Response to Request for Technical Assistance

Immigration Crackdown and Medicaid Cuts Put Millions at Risk

Will This Time be Different? Past Health Bills Hold Clues