
How Medicaid Cuts Could Force Millions Into Nursing Homes
If Federal Support Falls, States May Slash Home- and Community-Based Services — Pushing Vulnerable Americans Into Nursing Homes They Don’t Want or Need
Improving Care for Older Adults
Blog Post
For patients and their families, deciding if and where to go to a nursing home for care is a difficult and emotional decision. Since 2016, the Department of Veterans Affairs has been publishing star ratings of its own nursing homes to help Veterans make that decision. VA-owned nursing homes, called Community Living Centers (CLCs), are an important source of skilled nursing care for recently hospitalized Veterans.
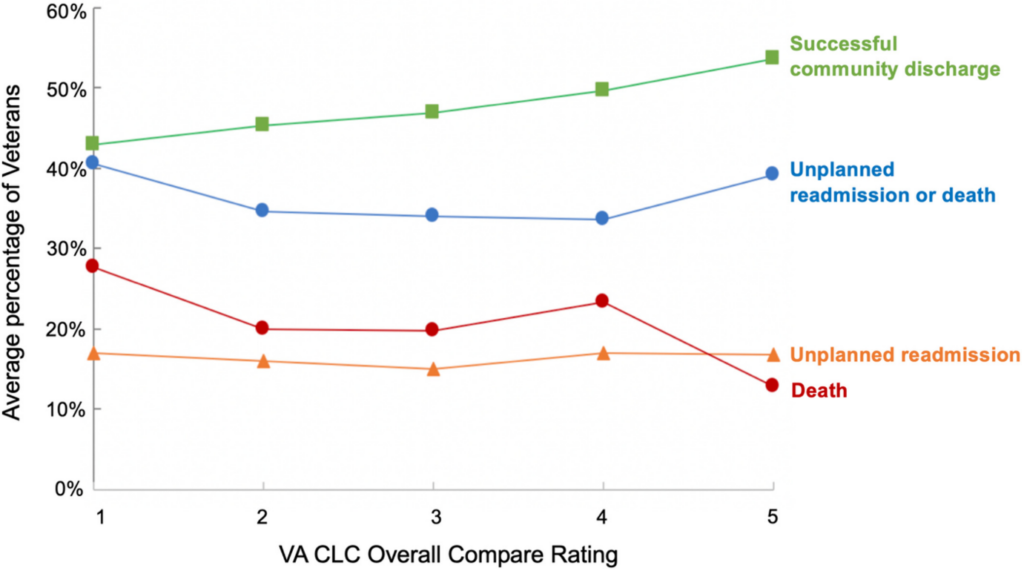
LDI Senior Fellows Mary Ersek and Robert Burke, along with their colleagues Kirstin Manges and Elina Medvedeva, recently published research testing whether these star ratings are linked to important quality indicators such as rates of unplanned readmission, successful discharge back to the community, and death for older Veterans admitted to a CLC for post-acute care.
The authors found that a 1-star rating was linked to lower quality outcomes, including a higher 30-day combined hospital readmission and/or death and a lower chance of successful discharge into the community, compared to high-quality five-star CLCs. However, star ratings of 2, 3, and 4 were not reliably linked to differences in quality.
What does this mean for consumers, particularly older Veterans seeking care from a CLC? The findings suggest that a low 1-star rating is an important signal of lower quality but that ratings in the middle of the scale may not translate to meaningful differences. The authors point out similar findings for a comparable nursing home rating system used by the Centers for Medicare and Medicaid Services. Going forward, the VA should identify what Veterans are looking for in a star rating measurement tool—and ensure that the ratings are clearly associated with quality outcomes—to better inform and empower consumer choice in care.
The study, VA Nursing Home Compare Metrics as an Indicator of Skilled Nursing Facility Quality for Veterans, was published in the June 9, 2022, issue of the Journal of the American Geriatrics Society. Authors include Kirstin A. Manges, Elina Medvedeva, Mary Ersek, and Robert E. Burke.

If Federal Support Falls, States May Slash Home- and Community-Based Services — Pushing Vulnerable Americans Into Nursing Homes They Don’t Want or Need

Men are Stepping Up at Home, but Caregiving Still Falls On Women and People of Color LDI Fellow Says

Economist Norma Coe’s Caregiving For Relatives Informed Her Research

The Decline Since 2020 May Signal Gaps in Service and Access

Penn Event Explores the Limits of Chronological Aging and Related Issues

LDI Executive Director Discusses New Findings on Medicare Beneficiaries’ Use of Home Health

The Tragic Deaths of the Actor With Dementia and His Wife Signal a System That Often Fails to Support Caregivers

Briefing: Presented to Staff of U.S. Senate Committee on Finance