Medicare’s Skilled Nursing Facility Value-Based Purchasing Program Fails to Lower Hospital Readmissions
Research Brief: New Incentive Structures and Metrics May Improve Program Performance
Blog Post
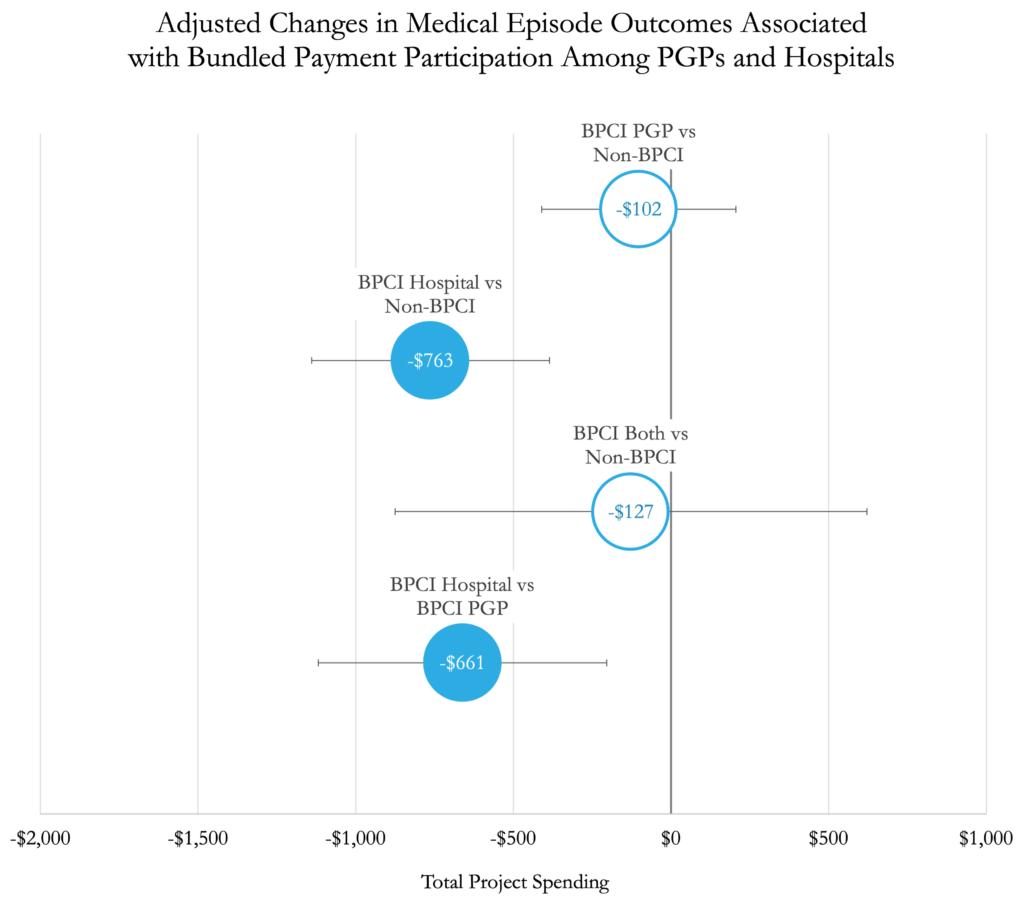
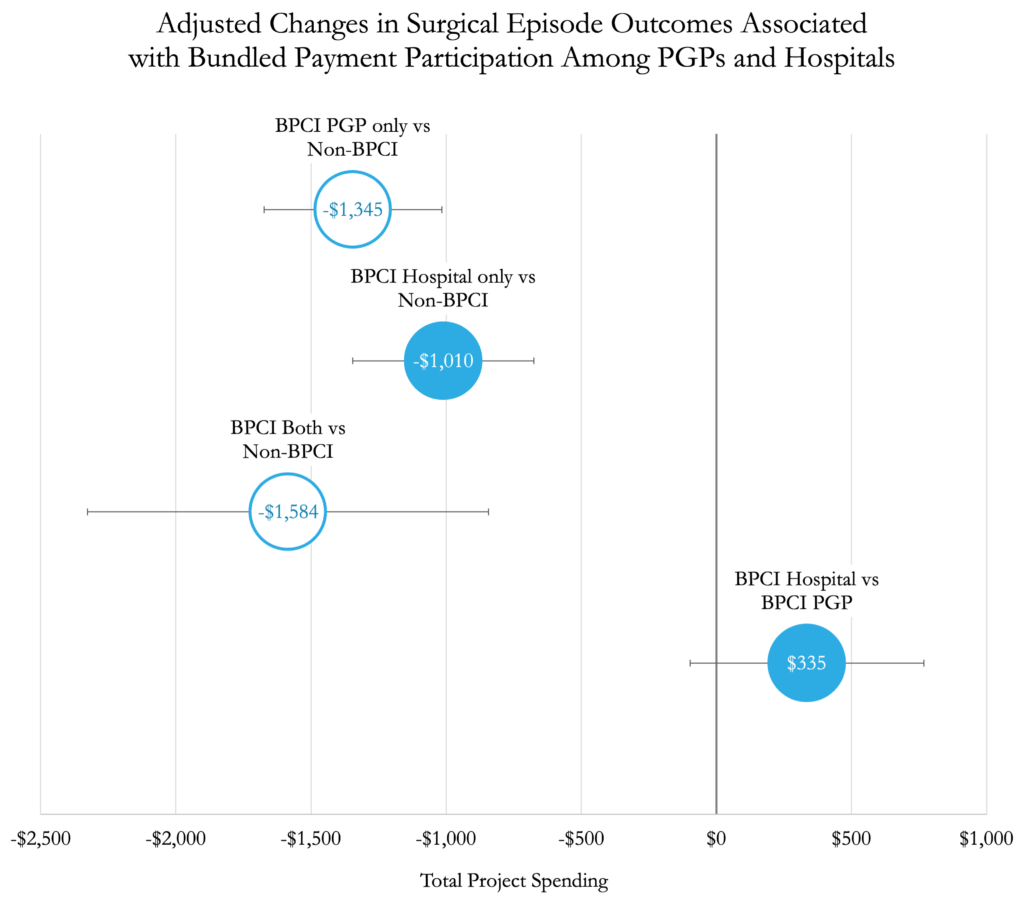
Bundled payments are a key strategy used by payers to reduce costs around episodes of care. However, little is known about how well physician group practices vs. hospitals perform when participating in these alternative payment models. Medicare’s Bundled Payments for Care Improvement (BPCI) program, which covers the costs of medical and surgical episodes from hospital admission for up to 90 days of post-acute care, offers an opportunity to answer this question.
In a new JAMA Health Forum study, LDI Adjunct Senior Fellow Joshua Liao, Senior Fellow Amol Navathe, and colleagues examine cost outcomes in physician groups and hospitals participating in the BPCI program.
After assessing claims data from over 1.2 million Medicare beneficiaries, they found that spending for surgical episodes decreased similarly for hospitals and physician groups. However, for medical episodes, only hospitals achieved significant reductions.
As policymakers and payers continue to design and evaluate bundled payment models, they should consider how the performance of participant types compares to others for various types of care. In this study, hospitals seemed better positioned to achieve savings in medical episodes while both were successful around surgical episodes.
The study, “Performance of Physician Groups and Hospitals Participating in Bundled Payments Among Medicare Beneficiaries,” was published on December 9, 2022, in JAMA Health Forum. Authors include Joshua Liao, Qian Huang, Erkuan Wang, Kristin Linn, Torrey Shirk, Jingsan Zhu, Deborah Cousins, and Amol Navathe.

Research Brief: New Incentive Structures and Metrics May Improve Program Performance

Research Memo: Response to Request for Technical Assistance

Immigration Crackdown and Medicaid Cuts Put Millions at Risk

Will This Time be Different? Past Health Bills Hold Clues

Research Memo: Supplement to Response to Request for Technical Assistance

Many With High Drug Costs Have Supplemental Coverage and Won’t Reach the $2,000 Out-of-Pocket Cap, a New LDI Study Finds