
A Hidden Threat After Cancer: Food Insecurity and Early Death
Food-Insecure Cancer Survivors Live Shorter Lives, Especially if They Can’t Use Federal Programs Like SNAP
Health Care Access & Coverage | Health Equity
A lower extremity amputation in a patient with peripheral artery disease—narrowing of the arteries that supply blood to the legs or feet—is the culmination of years of failure by the U.S. health system. Our study, published in the Journal of the American Heart Association, shows that all too frequently, these failures affect Black people and those of low socioeconomic status.
Amputation is the last step in a years-long process of the build-up of atherosclerotic plaque in the arteries of the lower extremity. Atherosclerotic plaque begins to develop in the teenage years, and progresses through young adulthood and into middle age. It is spurred on by well-known and treatable risk factors: high cholesterol, high blood pressure, smoking, diabetes, lack of physical activity. Eventually, arteries become so narrowed that patients may develop cramping and pain in their legs with walking. Ultimately, the narrowing can progress to the point that there is not enough blood supply to heal wounds and even a small cut on the foot can lead to infection and the need for amputation. At every stage along this decades-long journey, there are opportunities to intervene and stop or slow the progression to amputation.
Prior studies have shown that people living in rural areas, especially poor and non-white people, have higher rates of amputation. The lay press has also focused on this population. The prevailing hypothesis is that distance from subspecialty cardiovascular and peripheral artery disease care, which is concentrated in urban centers, represents a key barrier for these patients. However, less than 20% of Americans live in rural areas, and geographic distance is only one of a number of barriers to health care that may be faced by poor and non-white individuals.
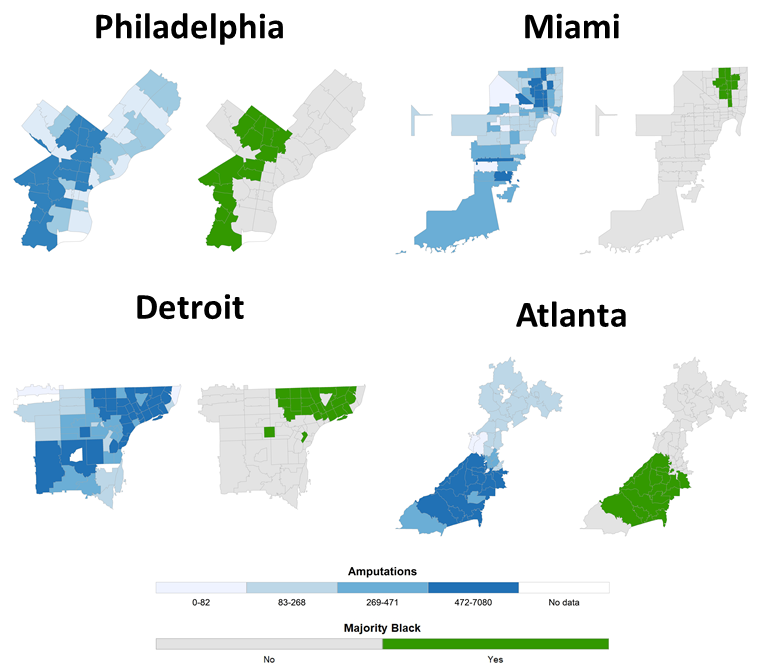
In our study, we looked at the rate of amputation per 100,000 Medicare beneficiaries in all U.S. ZIP codes. We found that ZIP codes with lower socioeconomic status or a greater proportion of Black residents had higher amputation rates than ZIP codes with higher socioeconomic status or a lower proportion of Black residents, whether these ZIP codes were urban or rural. When we mapped amputation rates, we found that high amputation rate ZIP codes colocalized with low income and majority Black ZIP codes (Figure 1). West Philadelphia, for example, has amputation rates comparable to those in rural Alabama, despite having a major medical center nearby.
In West Philadelphia, and similar communities in other American cities, geography may not be a barrier to excellent peripheral artery disease care, but barriers still exist. Peripheral artery disease progresses over a long time course, and barriers may exist at every stage of that process: inadequate referral rates to peripheral artery disease specialists, difficulty accessing pharmacy services or paying for prescriptions to treat vascular risk factors, lack of safe spaces to walk or buy fresh fruits and vegetables, and lack of education about the causes, symptoms, and treatment of peripheral artery disease. Investment in the development and implementation of scalable community-based resources, specifically targeted to urban communities with high amputation rates—such as community screening and education programs, home-based walking programs, and collaborative efforts to improve the quality of medical management in patients with or at risk for peripheral artery disease—are needed to dismantle these barriers. Importantly, 80% of individuals who undergo lower extremity amputation in the U.S. live in urban areas, highlighting the importance of developing programs specifically targeted to these communities.
The COVID-19 pandemic has highlighted the disparities in health outcomes in urban communities with low socioeconomic status and high proportions of Black residents, but these disparities existed long before the start of the pandemic. Taking these disparities seriously will require investments to rebuild systems of care that too often fail poor individuals living in urban areas.
The study, Geographic and Socioeconomic Disparities in Major Lower Extremity Amputation Rates in Metropolitan Areas, was published in the Journal of the American Heart Association on August 25, 2021. Authors include Alexander C. Fanaroff, Lin Yang, Ashwin S. Nathan, Sameed Ahmed M. Khatana, Howard Julien, Tracy Y. Wang, Ehrin J. Armstrong, Diane Treat‐Jacobson, Julia D. Glaser, Grace Wang, Scott M. Damrauer, Jay Giri, and Peter W. Groeneveld.


Food-Insecure Cancer Survivors Live Shorter Lives, Especially if They Can’t Use Federal Programs Like SNAP

Outdated Laws Target Black and Queer Lives in Over 30 States, Fueling a Deadly Disease

Selected for Current and Future Research in the Science of Amputee Care

Penn LDI Seminar Details How Administrative Barriers, Subsidy Rollbacks, and Work Requirements Will Block Life-Saving Care

Top Experts Warn of Devastating Impact on Community Safety Efforts

A Gathering of a Health Services Research Community Currently Under Siege