Medicare’s Skilled Nursing Facility Value-Based Purchasing Program Fails to Lower Hospital Readmissions
Research Brief: New Incentive Structures and Metrics May Improve Program Performance
Blog Post
Medicare Advantage (MA)–the private alternative to traditional Medicare–is now projected to enroll more than half of all Medicare recipients this year for the first time. The surge in MA plans has fueled concerns that the program is overfunded, and enables plans to grow by offering gym memberships, dental care, and other supplemental benefits.
Indeed, the Medicare Payment Advisory Commission found that MA plan payments were several percentage points higher than the expected spending of MA beneficiaries if they enrolled in traditional fee-for-service (FFS) Medicare.
Such concerns led researchers to wonder about the effects of future cuts on MA. Could those reductions cause unintended consequences, such as lower enrollment?
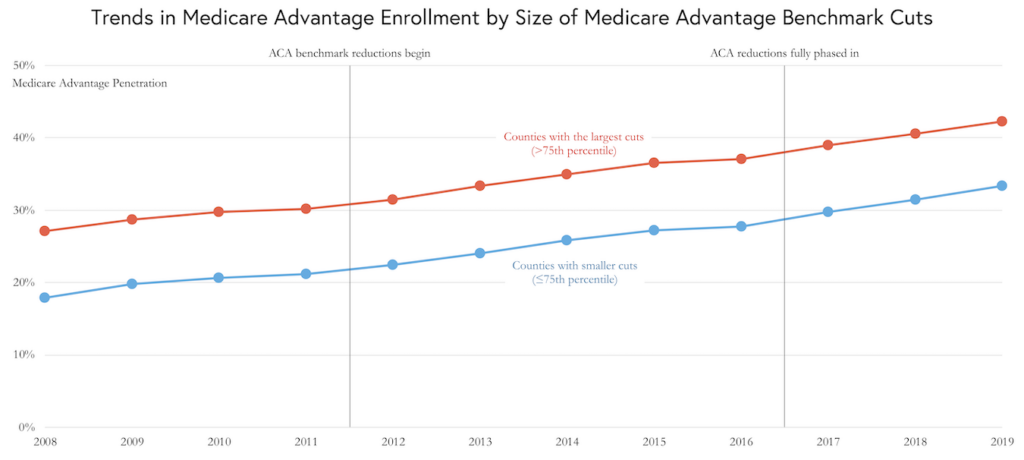
In a June study published in JAMA Health Forum, LDI Senior Fellows Aaron L. Schwartz, Amol S. Navathe, and Atul Gupta (with colleague Seyoun Kim) studied the Affordable Care Act’s (ACA) cuts to MA and whether those affected enrollment. The team looked at 3,138 counties for eight years after the ACA took effect, and found that counties with larger cuts to MA plans had similar enrollment growth as counties facing smaller cuts.
“This study extends prior research showing no immediate effects of the ACA on MA enrollment in the one year after ACA reforms,” the authors wrote. “One interpretation of these findings is that the MA program could absorb further payment cuts without shrinking the MA market.”
Still, the authors note, the effects of future MA payment reductions could differ even if they are of the same magnitude.
The study, “Growth of Medicare Advantage After Plan Payment Reductions,” was published on June 24, 2023 in JAMA Health Forum. Authors include Aaron L. Schwartz, Seyoun Kim, Amol S. Navathe, and Atul Gupta.

Research Brief: New Incentive Structures and Metrics May Improve Program Performance

Research Memo: Response to Request for Technical Assistance

Immigration Crackdown and Medicaid Cuts Put Millions at Risk

Will This Time be Different? Past Health Bills Hold Clues

Research Memo: Supplement to Response to Request for Technical Assistance

Many With High Drug Costs Have Supplemental Coverage and Won’t Reach the $2,000 Out-of-Pocket Cap, a New LDI Study Finds