
Experts: Medicaid Cuts Could Prove Fatal for Thousands
Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds
Blog Post
The idea of “nudges” to improve clinical decision-making is appealing, but which ones actually work? In a systematic review in BMJ Open, Briana Last, Alison Buttenheim, Nandita Mitra, Rinad Beidas, and colleagues find that the most effective nudges tend to be the most assertive ones, often changing default options or reducing decisions to a limited set of choices.
Nudges alter the way choices are presented, to overcome predictable errors in decision-making. They can be more or less potent, as shown in the “ladder” (Figure 1) based on Mitesh Patel’s adaptation of the Nuffield of Bioethics’ “intervention ladder.” Stronger interventions that limit clinicians’ choice are on higher rungs and more passive interventions that provide information or reminders are on lower rungs.
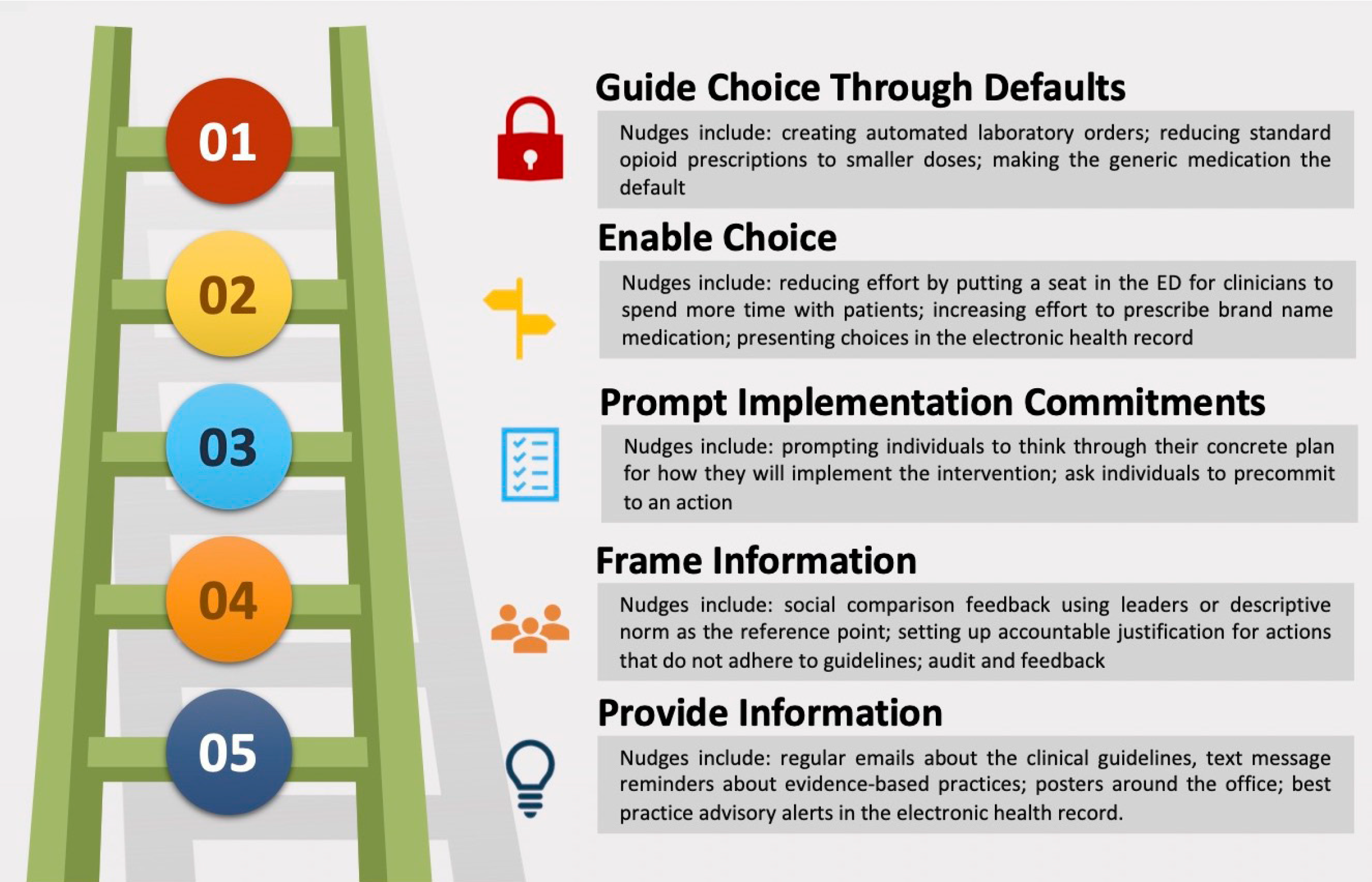
In their review of 39 studies, the authors found that nudges were generally effective: most nudges (73%) studied significantly improved clinical decisions. Nudges that changed default options (such as lowering the number of opioid prescription pills) or enabled choice through an “active opt-out” model were most effective. Nudges that framed information for clinicians (such as peer-comparison interventions) were also largely effective. On the other hand, nudges that provided information to the clinician through reminders did not significantly change clinician behavior.
As the world of behavioral economics and nudges continues to expand—just look to the Penn Medicine Nudge Unit—health systems and clinicians will need guidance on the type of nudge to implement, how to scale effective ones, and how nudges may interact in a clinical setting. This systematic review adds to the growing science around how nudges can improve clinical practice.
The study, Systematic Review of Clinician-Directed Nudges in Healthcare Contexts, was published in BMJ Open. Authors include Briana S. Last, Alison M. Buttenheim, Carter E. Timon, Nandita Mitra, and Rinad S. Beidas.


Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds

Cited for “Breaking New Ground” in the Field of Hospital Operations

Men are Stepping Up at Home, but Caregiving Still Falls On Women and People of Color LDI Fellow Says

More Flexible Methadone Take-Home Policy Improved Patient Autonomy

Penn LDI Seminar Details How Administrative Barriers, Subsidy Rollbacks, and Work Requirements Will Block Life-Saving Care

His data-driven initiatives risk violating consent, spreading stigma, and reviving vaccine misinformation, LDI Fellow writes.