
Estimated Overdose Deaths Due to the Loss of MOUD in the One Big Beautiful Bill Act
Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune
Blog Post
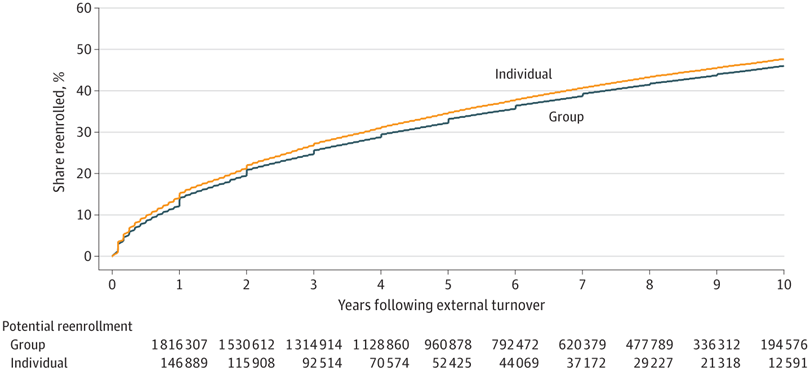
A recent study in JAMA Network Open measured and reported rates of disenrollment and reenrollment in commercial health plans. Using administrative data from Anthem, a large national insurer, Senior Fellow Hanming Fang, with former LDI colleagues Molly Frean and Benjamin Ukert, found that about one-third (34%) of members who leave their insurance plan reenroll with the same plan within five years. After 10 years, almost half (47%) were reenrolled. The findings were similar for those with individual and group insurance.
These data are important for insurance benefit design, and insurers may find it beneficial to factor reenrollment rates into policy decision-making. The findings suggest that insurers may benefit from focusing on the long-term health of members since many will return before long to the same insurer. In particular, such high rates of reenrollment may incentivize insurers to offer earlier preventive services since many members will likely be covered by the same insurer when the savings from such services will be realized.
The study, Trends in Disenrollment and Reenrollment Within U.S. Commercial Health Insurance Plans, 2006-2018 was published in JAMA Network Open on February 24, 2022. Authors include Hanming Fang, Molly Frean, Gosia Sylwestrzak, and Benjamin Ukert.
This research was made possible through an external research partnership between Penn LDI, the Wharton School Health Care Management Department, and Anthem Inc. This collaboration provides access to Anthem claims data and seeks to answer questions focused on using provider payment and insurance design to improve health care access, cost, and quality.

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Research Memo: Delivered to House Speaker Mike Johnson and Majority Leader John Thune

Historic Coverage Loss Could Cause Over 51,000 People to Lose Their Lives Each Year, New Analysis Finds
Research Brief: New Incentive Structures and Metrics May Improve Program Performance

Research Memo: Response to Request for Technical Assistance

Immigration Crackdown and Medicaid Cuts Put Millions at Risk

Will This Time be Different? Past Health Bills Hold Clues

Research Memo: Supplement to Response to Request for Technical Assistance