News
Penn Research Posters at 2017 AcademyHealth Annual Research Meeting
Photo Feature of Investigators and Their Work
As the U.S. political establishment continued its acrimonious debate over the direction of health care policy, more than 2,500 health services researchers assembled at the 2017 AcademyHealth Annual Research Meeting (ARM) in New Orleans to share their latest findings on how best to improve quality and lower costs of patient care. AcademyHealth is North America’s largest professional group of researchers focused on the organization, financing, management and delivery of health care. As usual, a sprawling section of the Research Meeting’s expo hall was devoted to a gallery of nearly 1,300 posters detailing research projects from across the country and the work of dozens of University of Pennsylvania scientists were included among them. Above in the Hyatt Regency Conference Center, Penn’s Ellen McGeoch and Sajal Kulhari hang their project poster. McGeoch, MS, is a Project Manager at Penn’s Leonard Davis Institute of Health Economics (LDI); Kulhari, BS, is an LDI Research Assistant. Their poster details a study entitled “Optimizing Your Shopping Cart: Decision Support Tools and Plan Presentation on the Health Insurance Market Place.” The work was a survey and overview of how the “choice architecture” features and functions of twelve state health insurance exchanges and HealthCare.gov have evolved over the last three years. Co-investigators included LDI Senior Fellows Daniel Polsky, PhD; Janet Weiner, PhD, MPH; Tom Baker, JD; and Charlene Wong, MD, former LDI Fellow and now an Assistant Professor at Duke University School of Medicine.
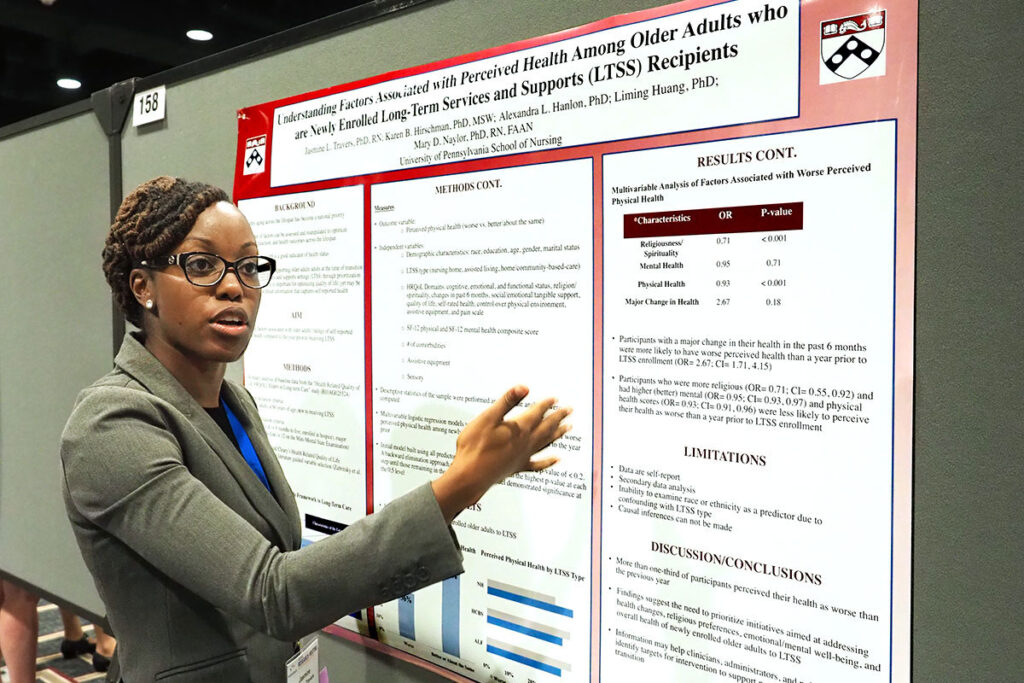
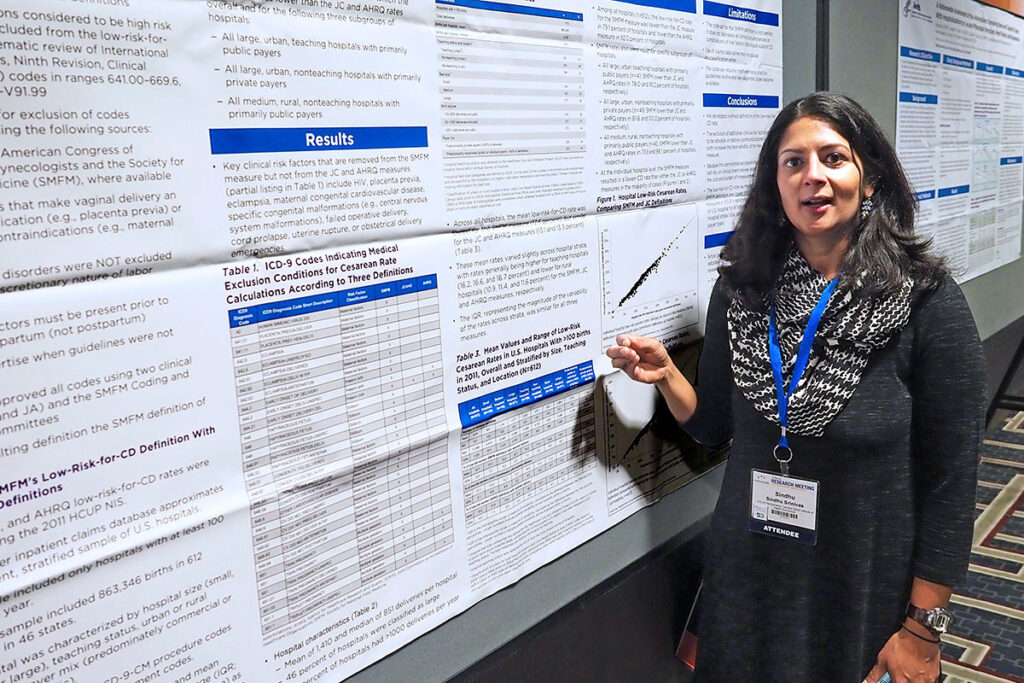
(Above, left) Penn Nursing School Postdoctoral Fellow and LDI Fellow Jasmine Travers, PhD, AGNP-C, RN, CCRN, details her study entitled “Understanding Factors Associated with Perceived Health Among Older Adults Who Are Newly Enrolled Long-Term Services and Support (LTSS) Recipients.” The project focused on how older adults in nursing homes, assisted living facilities and home & community-based services perceived how their health had changed in those institutions. More than a third believed their health had worsened. LDI Senior Fellow Mary Naylor, PhD, RN, FAAN, was a co-investigator. (Above, right) Perelman School of Medicine Associate Professor and LDI Senior Fellow Sindhu Srinvas, MD, MSCE, explained her team’s work that was a Healthcare Cost & Utilization Project (HCUP) Outstanding Article of the Year Award winner. It’s entitled, “Comparing Variation in Hospital Rates of Cesarean Delivery Among Low-Risk Women Using Three Different Measures.”
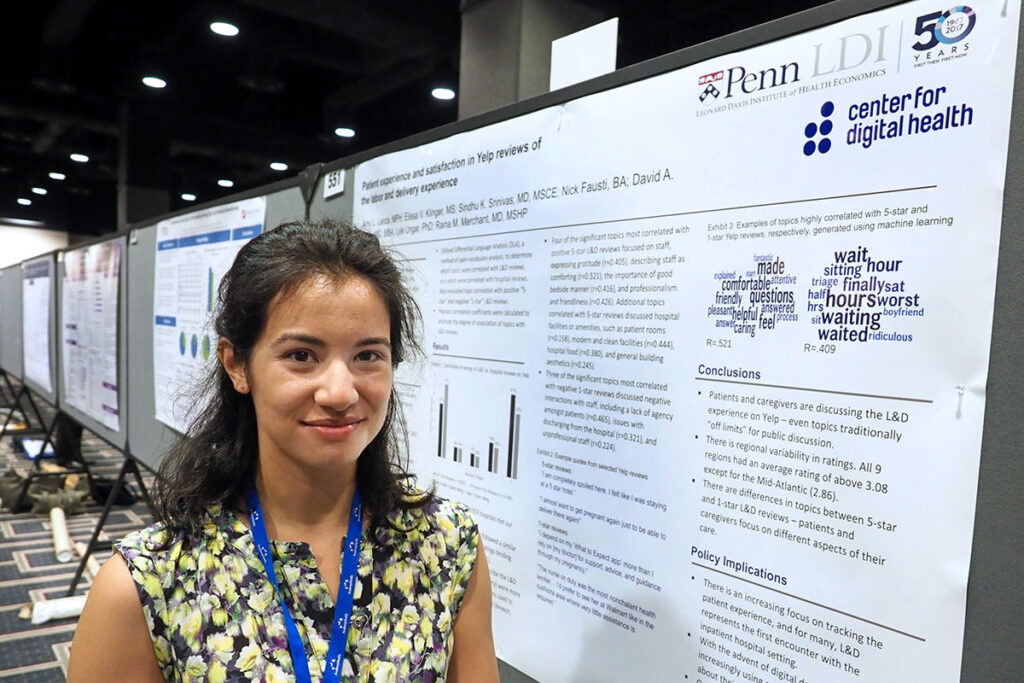
(Above, left) Penn Medicine Center for Health Care Innovation Research Coordinator Amy Lanza, MPH, was the primary investigator on this Center for Digital Health study of maternity patients’ Yelp.com reviews of their OB/GYN-related care. It is entitled, “Patient Experience and Satisfaction in Yelp Reviews of Obstetric and Gynecologic Care.” The research team found that online reviews can provide meaningful information about patient satisfaction and experience that are not captured in standardized, nationwide hospital surveys and can inform benchmarking of care for specialized areas like OB/GYN. Co-investigators included LDI Senior Fellows Sindhu Srinvas, MD, MSCE; David Asch, MD; and Raina Merchant, MD. (Above, right) Penn medical student and Research Assistant at the Center for Health Incentives and Behavioral Economics (CHIBE) Alexander Bain discussed his poster with Eugene Rich, MD, of Mathematica Policy Research. Entitled, “Relationship of Process Measure Improvements to System Outcomes and Savings in Accountable Care Organizations,” the work focused on evaluating how baseline performance and improvement on Accountable Care Organization process measures might be associated with other measures of ACO performance. Co-investigators included LDI Fellow Joshua Liao, MD; and LDI Senior Fellow Amol Navathe, MD, PhD.
(Above, left) Tending her poster about a joint study of Penn’s Department of Emergency Medicine and the CHERISH Center (Center for Health Economics Treatment Interventions for Substance Use Disorder, HCV and HIV) is Penn med student and primary investigator Rachel Graves, BS. Entitled “Pharmacist Knowledge of Naloxone Standing Order and Naloxone Availability in Pennsylvania Pharmacies,” the project found that fewer than 50% of pharmacies in Pennsylvania carried the opioid-overdose-reversing drug Naloxone despite the fact that the CDC ranks the state 8th in total number of annual drug overdose deaths. Co-investigators included LDI Senior Fellows Zachary Meisel, MD, and Raina Merchant, MD. (Above, right) Ellen McGeoch, MS, explains her second study poster to Brian McGarry, PhD, a Research Fellow in Health Care Policy at Harvard Medical School.. Entitled “What’s the Bottom Line? Total Cost Estimators on the Health Insurance Marketplace,” the study analyzed the calculation tools on public and private health insurance exchanges in twelve states and HealthCare.gov. It found that on average, the public exchange estimates were $867 lower than the private exchange estimates for the same plan. Co-investigators included LDI Senior Fellows Janet Weiner, PhD, MPH and Daniel Polsky, PhD.
(Above, left) Fourth year Wharton School Health Care Management PhD student Amelia Bond, MHS, discusses her poster detail with Junling Wang, PhD, Professor of Clinical Pharmacy at the University of Tennessee. Entitled, “Real-Time Feedback in Pay-for-Performance: Does More Information Lead to Improvement?,” the study analyzed the effect of enabling physicians working in a pay-for-performance reimbursement program to see their quality scores in real-time rather than once a quarter. The research team found that real-time quality reports were insufficient to improve physician performance within an existing P4P program. Co-investigators included LDI Senior Fellows Kevin Volpp, MD, PhD; Ezekiel Emanuel, MD, PhD; and Amol Navathe, MD, PhD. (Above, right) Perelman School of Medicine Pulmonary and Critical Care Medicine Fellow and LDI Fellow Gary Weissman, MD, discusses the benefits of including data from physicians’ notes in clinical predictive models with Wenke Hwang, PhD, of Penn State College of Medicine. Entitled “Inclusion of Unstructured Text Data from Clinical Notes Improves Early Prediction of Death or Prolonged Intensive Care Unit Stay Among Hospital Patients,” Weissman’s poster details a study that showed how use of unstructured narrative data harvested from physician notes in electronic medical records improved the accuracy of various clinical predictive models. Co-investigators included LDI Fellow Michael Harhay, MPH, and LDI Senior Fellow Scott Halpern, MD, PhD.
(Above, left) Perelman School Fellow in Pulmonary & Critical Care and LDI Fellow Rachel Kohn, MD, attends her poster that details a study she conducted of ward capacity strain and its patient care effects. The discharge of various volumes of intensive care unit survivors into general hospital wards can create a capacity strain that could impact those survivors’ ultimate care and outcomes. This study was aimed at analyzing the drivers and dynamics of ward strain in more than two dozen wards in three Pennsylvania hospitals. The title of the study is “Ward Capacity Strain: Defining a New Construct Based on Emergency Department Boarding Time and Intensive Care Unit Transfers.” (Above, right) Perelman Associate Professor of Medicine and LDI Senior Fellow Bruce Kinosian, MD, was part of a study that looked at the comparative costs and care quality of using home and community-based care services for frail veterans’ long-term care. The poster is entitled “Veterans Health Affairs Geriatrics and Extended Care Bending the Cost Curve: Evidence and Challenges” and concludes there was a small savings per year achieved through this care model.
(Above, left) Penn School of Nursing Associate Professor and NewCourtland Term Chair in Health Transitions Research Karen Hirschman, PhD, MSW, explains her poster entitled “Cost Impact on the Transitional Care Model for Hospitalized Cognitively Impaired Older Adults.” The study compared the costs and effects of three different transitional interventions led by advance practice registered nurses; two in hospital settings and one in a hospital-to-home settings. All involved cognitively impaired high-risk elderly patients. Results were that the APRN model of care lowered the cost on both acute care and total hospitalization-post-discharge. Co-investigators included LDI Senior Fellows Mark Pauly, PhD; Kathryn Bowles, PhD, RN, FAAN; and Mary Naylor, PhD, RN, FAAN. (Above, right) Clinical Research Coordinator at the LDI Center for Health Incentives & Behavioral Economics (CHIBE) Kristen Caldarella, MHA, tends a poster detailing “A Randomized Trial of Using Loss Aversion and Enhancing Group-Based Incentives in a Physician Pay-for-Performance Program.” The study tested the impact of loss aversion and social pressure behavioral economics principles on the quality of the pay-for-performance work of physicians in primary care and specialist practices in Chicago. The researchers reported positive results that will be useful in further determining how to design more effective P4P incentive systems. Co-investigators included LDI Senior Fellows Amol Navathe, MD, PhD; Ezekiel Emanuel, MD, PhD; Kevin Volpp, MD, PhD.
(Above, left) Robert Wood Johnson Foundation Clinical Research Scholar at the Veterans Administration and LDI Fellow Manik Chhabra, MD, mans a poster entitled “Implementation of a Payer-Led, Practice Based Care Management Program for High-Cost, High Need Patients.” The study analyzed the cost and quality impacts of embedding payer management teams at clinical practice sites involved in the care for high-cost, high-need patient populations. Researchers found that legal obstacles that resulted in duplicate processes and delayed information sharing were major challenges to the operation of such partnerships. Co-investigators included LDI Fellow Krisda Chaiyachati, MD, MPH; and LDI Senior Fellows David Grande, MD and Judy Shea, PhD. (Above, right) Penn Nursing doctoral student Ashley Ritter, MSN, CRNP, is with a poster of her study, “Deconstructing Nurse Practitioner (NP) Collaborative Practice Agreements: Occupational Licensure and Competition.” The work analyzed the effect of mandated collaborative agreements between nurse practitioners and physicians in states where laws require such NP practice restrictions. Researchers concluded that legally required collaborative agreements disrupt competitive market forces with questionable consumer protection benefits. Co-investigators included LDI Senior Fellows Kathryn Bowles, PhD, RN, FAAN, and Julie Fairman, PhD, FAAN.
(Above, left) Fellow in Gastroenterology at the Perelman School of Medicine and LDI Fellow, Shazia Mehmood Siddique, MD, discusses her poster that documents a project creating the Carelign web platform that supports a more integrated method for sharing patient information among clinicians: “Carelign: A Novel Tool for Closing the Loop on Inpatient Consultant Communications.” (She’s speaking with Brian Leas, MS, of Penn’s Center for Evidence-Based Practice). Linked to a mobile application and integrated into the health system’s EPIC electronic health records system, the Carelign system functions as a single portal in which primary and consulting clinical teams can access and enter patient information and recommendations in real time. A co-investigator was LDI Fellow Srinath Adusumalli, MD. (Above, right) Rutgers School of Nursing Assistant Professor Olga Jarrin, PhD, RN, discusses a Penn Nursing School Center for Health Outcomes and Policy Research project entitled, “Hospital Admissions Associated With Home Health Agency Management.” The study was focused on 426 home health care agencies in four states and the evaluation of the relationship between agency management, nursing care quality and patient outcomes. It is the first study to investigate the effects of agency management on hospital utilization. It found that agencies rated as having the best management in the CMS Home Health Compare database were nearly half as likely to have an elevated rate of acute care hospitalizations. They were also more than five times more likely to have nurses say they always had time to complete necessary patient care and care coordination tasks than agencies rated as having the worse management. Co-investigators included LDI Senior Fellows Matthew McHugh, PhD, JD, MPH and Linda Aiken, PhD, RN.