
Experts Warn Addiction Policy is Weak Despite Falling Overdose Deaths
Penn LDI Panel Urges Family-Focused Strategy and Stronger Health System Response
Blog Post

For the more than 80,000 people in the U.S. who will test positive for COVID-19 today, how can we offer access to health care and help them safely remain at home?
When the pandemic started, our team at Penn Medicine designed COVID Watch, an automated text-messaging service to manage COVID-19 patients and relieve pressure on emergency departments. Our goal was to facilitate hospital care for patients who require it while supporting access to care for patients who could safely remain at home. According to findings we just published in Annals of Internal Medicine, COVID Watch reduced mortality among patients with COVID-19, likely by getting them to the emergency department (ED) more often and earlier.
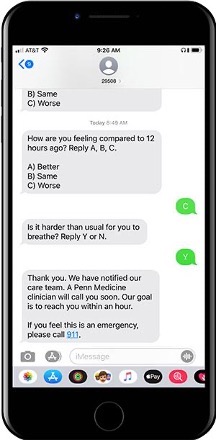
We analyzed data from 7,825 University of Pennsylvania Health System (UPHS) patients who tested positive for COVID-19 outside the hospital from March 21 to November 30, 2020. Of these, 4,377 patients received usual care, which meant they were responsible for seeking treatment for their symptoms via usual methods (calling or messaging their doctor if they have one, or making their decision on their own to go to the ED). In contrast, the 3,488 COVID Watch patients received automated text check-ins twice a day. If they indicated difficulty breathing, nurses called and assessed them, on average within 30 minutes. Based on their conversation, patients either continued to self-monitor at home, were directed to the ED, or set up with an urgent telemedicine appointment.
COVID Watch patients were similar in age to those who received usual care but were more likely to be female (43% vs. 37%); Black (48% vs. 32%); have public insurance (29% vs. 27%); not have a primary care provider (28% vs. 25%) and live in poorer neighborhoods (median annual income $51,000 vs. $61,000).
Using data in the electronic medical record (test date, demographics, clinical characteristics, prior health care use, home ZIP code,) we balanced baseline patient characteristics to make accurate comparisons between COVID Watch and usual care patients.
We found that overall mortality was less than 1% in both groups at 60 days. However, five of 3,448 (0.14%) COVID Watch patients died compared to 16 of 4,377 (0.37%) patients who received usual care. After risk adjustment, this is 2.5 fewer deaths per 1,000 patients enrolled and a 66% lower odds of death.
A second finding was that six of 16 (38%) of deaths in the usual care patients occurred outside the hospital versus none among COVID Watch enrollees. This suggests a key to this program was addressing fear about seeking ED care during the first wave of the pandemic. The main mechanism of benefit was that COVID Watch patients were more likely to present to the ED and when they did, they came in earlier – at the first sign of worsening breathing. Looking at all ED visits, they came in two days earlier and patients who came to a UPHS ED who required life-saving dexamethasone got it three days earlier, in time for it to have the most benefit.
Of note, over 50% of the patients enrolled in COVID Watch were Black or Hispanic and all major racial and ethnic subgroups had reduced mortality rates when enrolled in COVID Watch. This finding suggests that a text-based monitoring program could play a role in decreasing COVID-19 disparities.
COVID Watch saved lives by facilitating quicker presentation to the ED where treatment can be more effective if started earlier. This low-tech solution helped patients obtain hospital treatment when they needed it, without potentially fatal delays. These findings reinforce the value of emergency care in our health care system. During the pandemic, patients were fearful of seeking care in the ED, even for life-threatening conditions. COVID Watch helped overcome hesitancy by guiding patients to the ED at the right time. The findings also offer a caution to policies that seek to discourage patients from seeking emergency care, by putting them at risk for higher potential out-of-pocket costs if the final diagnosis is considered by an insurer to be “non-emergent.”
Finally, our work could have major implications for the future of health care after the pandemic. Automation, in the form of a simple text messaging system backed by a team of clinicians, could efficiently deliver care for large populations while improving their health. As we wrote on STAT,
“How our experience with Covid Watch can be applied to other acute needs like asthma or chronic obstructive pulmonary disease, or more chronic conditions such as diabetes or opioid use disorder, remains to be seen. But we believe that what we built — and the lives it saved — provides direction for how health care should be changing.”
The study, Comparative Effectiveness of an Automated Text Messaging Service for Monitoring COVID-19 at Home was published in Annals of Internal Medicine on November 16, 2021. The authors include M. Kit Delgado, Anna U. Morgan, David A. Asch, Ruiying Xiong, Austin S. Kilaru, Kathleen C. Lee, David Do, Ari B. Friedman, Zachary F. Meisel, Christopher K. Snider, Doreen Lam, Andrew Parambath, Christian Wood, Chidinma M. Wilson, Michael Perez, Deena L. Chisholm, Sheila Kelly, Christina J. O’Malley, Nancy Mannion, Ann Marie Huffenberger, Susan McGinley, Mohan Balachandran, Neda Khan, Nandita Mitra, and Krisda H. Chaiyachati.




Penn LDI Panel Urges Family-Focused Strategy and Stronger Health System Response

Remote Nurses Improved Quality Slightly but Can’t Replace Nurses at the Bedside, a New Study Finds

Washington State’s First-in-the-Nation Insurance Plan Begins Payouts in Mid-2026, and Researchers Will Weigh its Effect on Care, Costs, and the Long-Term Care Markets

Without Pressure From Congress, NHANES — Which Helped Uncover High Levels of Childhood Lead, Nutritional Deficiencies, and Forever Chemicals — Will Cease to Exist

A Multi-State Study Finds That Parents Often Travel 60+ Miles—With Distance, Insurance, and Race Driving Gaps in Maternal Care

Former CMMI Leader Liz Fowler Cites Rigid Federal Scoring Rules and Bureaucratic Impatience for Pilot Failures

A Major European–U.S. Hospital Study Finds That Changing How Hospitals Are Organized Reduces Burnout and Turnover While Improving Care Quality

An LDI Fellow Who Helped Architect the ACA Highlights Progress on Primary Care Payment Reform and the Expansion of Site-Neutral Reimbursement Policies