
How Hospitals Can Ease Staff Burnout—and Improve Patient Safety
A Major European–U.S. Hospital Study Finds That Changing How Hospitals Are Organized Reduces Burnout and Turnover While Improving Care Quality
Blog Post

This year, LDI highlighted groundbreaking research by our Fellows, provided critical policy analyses, and distilled complex ideas into digestible insights for you, our readers. Thank you for joining us on this journey through the dynamic landscape of health policy in 2024!
Among the research updates we shared, some resonated particularly strongly with our audience. These pieces highlighted issues ranging from health care disparities and systemic racism to the financial challenges facing patients and the broader implications of health care system changes.
Here are 12 studies on crucial areas of health policy that captured your attention and sparked important conversations this past year:

Penn Study in Navajo Nation Boosts Guideline Heart Failure Drug Uptake by 53%
A simple telehealth-based strategy resulted in a 53% increase in the use of guideline-recommended medications for heart failure at a Navajo Nation hospital in New Mexico. The study led by Senior Fellow Lauren Eberly highlighted the impact of tailored interventions in improving cardiovascular care in underserved populations.

Research Brief: What Happens When a Multihospital System Buys an Independent Hospital?
LDI Fellows Atul Gupta and Catherine Ishitani examined the effects of independent hospitals being acquired by multihospital systems, finding that these acquisitions often lead to higher prices for care without clear improvements in quality.

Enrollment Grows in Integrated Managed Care Plans for Dual-Eligible Nursing Home Residents
LDI Senior Fellow Eric T. Roberts and Executive Director Rachel M. Werner conducted a first-of-its-kind examination of trends in the enrollment of dual-eligible nursing home residents into specialized managed care plans, finding that while more individuals are choosing such plans, overall enrollment remains low.

Racism Prematurely Ages Black People
Research by LDI Senior Fellow Courtney Boen revealed how systemic racism accelerates biological aging in Black Americans, exacerbating health disparities and shortening lifespans.

An analysis on historical billing practices conducted by Senior Fellow Atul Gupta found that for-profit hospitals were more likely than nonprofit hospitals to exploit Medicare outlier payments, raising concerns about aggressive billing practices and their implications for health care costs.

LDI Senior Fellows Katherine Courtright, Dylan Small, Mary Ersek, and Scott D. Halpern found that use of default orders in hospital systems significantly increased palliative care consultations for older patients. While there was no decrease in the length of stay, the study demonstrated that the default order could improve end-of-life care for seriously ill patients.

Many Medicare Beneficiaries Are One Hospital Visit Away from Poverty
LDI Senior Fellows Paula Chatterjee and Eric T. Roberts revealed that a single hospital visit can push many Medicare beneficiaries into poverty, highlighting the financial vulnerability of older adults and the need for policy solutions.

Do Wealth and Poverty Affect Access to Less-Invasive Cardiac Surgery?
By exploring how socioeconomic factors influence access to advanced cardiac procedures, Senior Fellows Guy David and Alon Bergman found that wealthier patients are more likely to receive less-invasive surgeries, highlighting disparities in health care access.

Medicaid expansion led to wage increases for higher-paid health care workers, such as doctors, nurses, and managers, while wages for lower-paid workers remained stagnant, according to research by LDI Fellows Sasmira Matta, Paula Chatterjee, and Atheendar Venkataramani. The finding highlighted disparities in economic benefits across the health care workforce.

Research by LDI Senior Fellows Jane M. Zhu and Marissa King illustrated significant state-by-state differences in private equity ownership of mental health and substance use disorder facilities, raising concerns about care quality and accessibility.

How Do Ownership Changes Affect Nursing Home Quality?
Senior Fellow Kira L. Ryskina and Executive Director Rachel M. Werner assessed the effects of nursing home ownership changes, finding that new ownership often leads to declines in quality measures. The finding raised concerns about the impact of ownership transitions on resident care and outcomes.
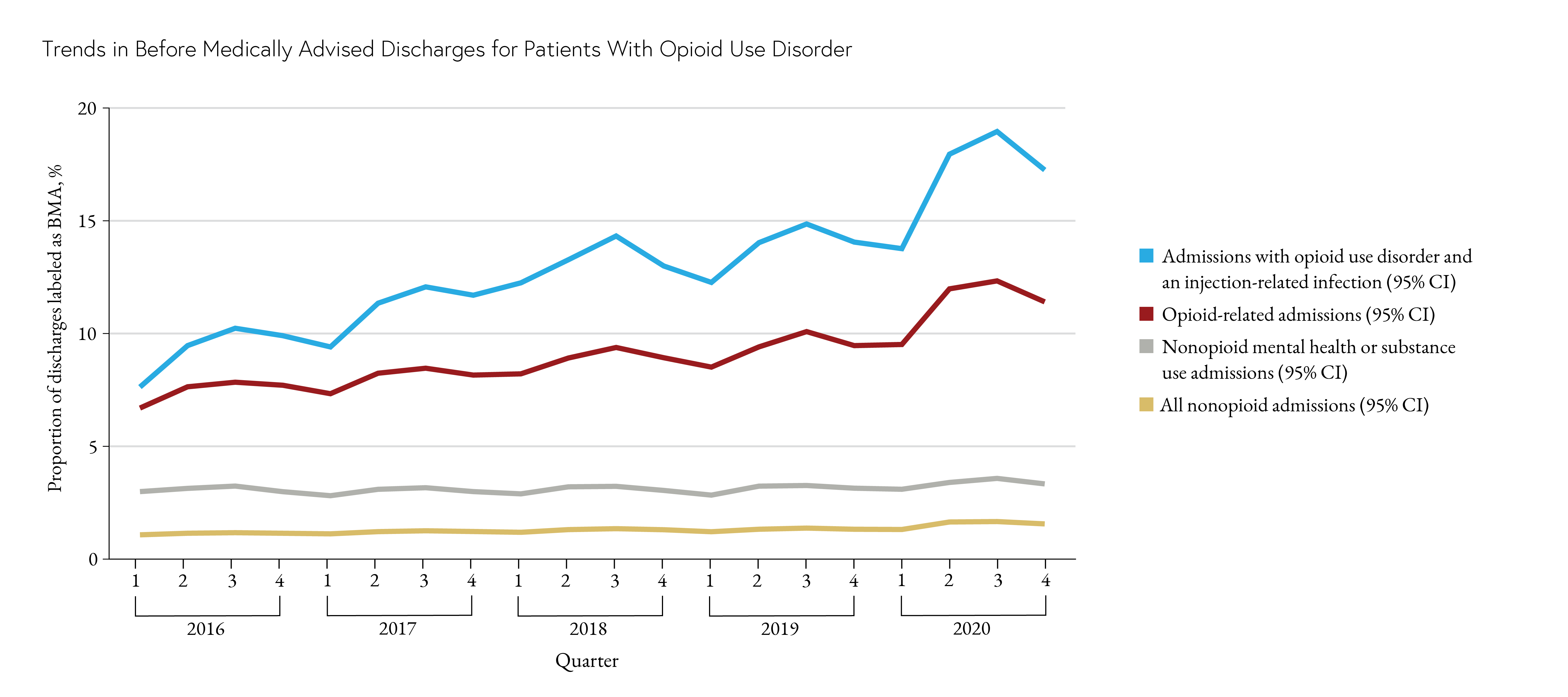
Chart of the Day: Rise in Patients with Opioid Use Disorder Leaving Hospital Prematurely
LDI Senior Fellows Ashish Thakrar, Margaret Lowenstein, Ryan Greysen, and Kit Delgado tracked a concerning rise in opioid use disorder among patients leaving hospitals prematurely, emphasizing the need for tailored interventions to support this vulnerable group.
Also see Top LDI News stories of the past year.


A Major European–U.S. Hospital Study Finds That Changing How Hospitals Are Organized Reduces Burnout and Turnover While Improving Care Quality

Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
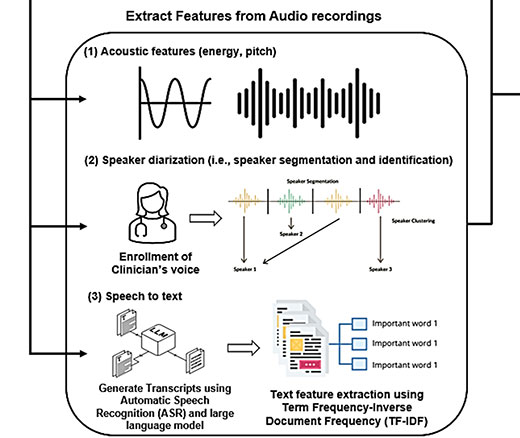
Researchers Use AI to Analyze Patient Phone Calls for Vocal Cues Predicting Palliative Care Acceptance

LDI Fellows’ Research Quantifies the Effects of High Health Care Costs for Consumers and Shines Light on Several Drivers of High U.S. Health Care Costs

A Licensure Model May Offer Safer Oversight as Clinical AI Grows More Complex, a Penn LDI Doctor Says

CF Foundation’s Landmark Drug Approvals With Vertex Inspired Patient Groups to Act Like Biotech Investors. But Only a Few Groups Have Made Big Bets, LDI Fellow Finds