
Black Older Adults With Cancer Are Far Less Likely to Get Any Care
New Study From LDI and MD Anderson Finds That Black and Low-Income, Dually Eligible Medicare Patients Are Among the Most Neglected in Cancer Care
Health Care Payment and Financing
Blog Post

Medicare will launch a new – and mandatory – bundled payment model, the Transforming Episode Accountability Model (TEAM), in 2026. The model will randomly select hospitals to participate, with episode-based payments for five surgical conditions: lower extremity joint replacement, spinal fusion, hip fracture, coronary artery bypass graft surgery, and major bowel procedures.
Given that Medicare has previously tested multiple bundled payment programs, what can we learn from TEAM in the coming years? The answer – a great deal. Bundled payments – where insurers set a target price for a health care service and follow-up period – remain the most promising way to hold specialists accountable through value-based care, and few other alternative payment models focus on acute, hospital-based care. Yet while these programs reduce spending for healthcare episodes, bonuses have resulted in net losses to Medicare, requiring adjustment of target prices. In addition, the impact of bundled payments on health disparities –for both access and outcomes – is complex. And it remains unclear which types of conditions – surgical or medical – work best for these models.
Our team at The Parity Center, which focuses on payment policy and health equity, sought to answer key questions for the future of bundled payments in two recent publications in JAMA Health Forum.
First, which can have the greatest impact on spending or quality, hospitals or physician groups? Our research suggests that both can perform well in these models, and physicians may have some advantages over hospitals.
Second, can bundled payments be effective for outpatient surgical procedures, beyond inpatient surgical procedures or medical admissions? In our analysis of the first Medicare bundled payment program for outpatient surgery, we found that spending fell, due to a surprising reduction in return admissions.
Our two studies — described in more detail below — should inform the evolution of the new TEAM model as well as future refinement of this essential strategy for payment reform.
Bundled payments are among the most well-studied forms of value-based payment. The concept is deceptively simple: set a target price for all services delivered within an episode of care, such as a surgical procedure and additional care delivered over the next 90 days. Participants, including hospitals and physicians, earn bonuses or accrue penalties depending on whether spending falls below or exceeds the target. In general, bundled payments have reduced spending before bonuses while maintaining quality, most notably for orthopedic procedures.
We answered these questions by examining an ongoing Medicare program, Bundled Payments for Care Improvement (BPCI) Advanced. Prior bundled payment models, including BPCI Advanced, have allowed both hospitals and physician groups to participate in the model. Hospitals or physicians can be an accountable entity for the episode of care, with the ability to earn bonuses and risk of accruing penalties. For some conditions, physician groups have been responsible for the vast majority of episodes (Figure 1). However, TEAM will only allow hospitals to enroll as direct participants.
We wanted to understand the impact of this policy change by examining the performance of physician groups in BPCI Advanced for the most common surgical procedure – lower extremity joint replacement.
Our study mentioned above was the first to include physician groups in an evaluation of BPCI Advanced. We analyzed the outcomes of over 800,000 Medicare beneficiaries who received joint replacement surgery. We found that surgeries performed by a physician in BPCI Advanced had a 3% reduction in episode spending, while surgeries at a participating hospital had 2% less spending. We also found evidence of synergy – participating surgeons operating at participating hospitals had 4% less spending per episode.
These findings suggest that physicians can perform comparably to hospitals in bundled payment models. In fact, physicians may have certain advantages over hospitals in improving quality and care coordination across an episode of care.
For example, participating surgeons may be incentivized to ensure that patients attend follow-up appointments after they are discharged home to prevent complications and ensure continuing recovery. For hospitals, ensuring that same follow-up care may be more challenging.
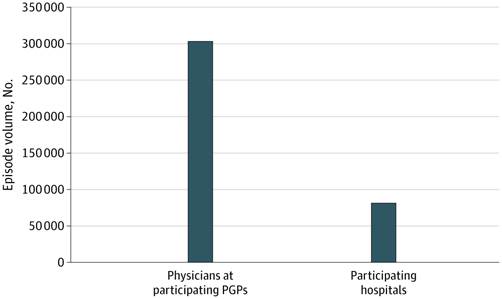
Figure 1. Total Volume of Joint Replacement Episodes Performed by Physician Group Practices (PGPs) and Hospitals Participating in BPCI Advanced. Source: Crowley et al. (2025). JAMA Health Forum.
Because of its mandatory design, it was likely infeasible to require physician groups to participate in the TEAM model. Yet one important aspect of the new model are mechanisms to help align incentives for participating hospitals and physician groups.
One approach is gainsharing – the ability for hospitals to share bonuses with physicians, even if those physicians are not employed by the hospital. Our study suggests that it will be important for TEAM participants to adopt gainsharing strategies, to ensure that physicians and hospitals share motivation to improve quality and cost-efficiency for patients. We encourage CMS to develop more specific guidance for hospitals on the best way to engage physicians in the bundled payment program.
Traditionally, bundled payments have been used for conditions that required either inpatient medical admission, like heart failure, or inpatient surgical admission. However, an increasing number of surgeries have been moved to the outpatient setting. Outpatient surgeries may be performed in a hospital or alternative setting, such as an ambulatory surgery center. Patients may still require a short period of hospitalization but are discharged soon after their procedure. BPCI Advanced was the first to include outpatient episodes in the model, including joint replacement, spine surgery (back and neck procedures that did not involve spinal fusion), defibrillator placement, and percutaneous coronary intervention.
There is real doubt about whether bundled payments for outpatient surgery can achieve spending or quality gains. The reason – bundled payments typically achieve savings by reducing the use of post-acute care, such as stays in skilled nursing facilities after hospital discharge. But post-acute care is typically not available after outpatient surgery. There has been almost no evidence to support the inclusion of outpatient surgery in bundled payment models.
Our next study was the first to examine outpatient surgery in a Medicare bundled payment model. We focused on spine surgery as an example of the newly included conditions. We examined outcomes of 14,280 Medicare beneficiaries who received outpatient spine surgery to see if hospital participation in BPCI Advanced was associated with changes in spending and quality. We were surprised to find that obtaining outpatient spine surgery at a participating hospital was associated with a 10% reduction in spending.
From where did those savings arise, if not reductions in post-acute care? We found a corresponding 30% reduction in return hospital admissions. These findings suggest that surgeries performed in the outpatient setting may benefit from incentives to redesign care – such as improving care coordination and other mechanisms to manage any subsequent complications in the outpatient setting.
Our findings were preliminary, given that we only examined one condition in the first two years of the BPCI Advanced program. Regardless, this study supports the decision for the TEAM model to include outpatient conditions. TEAM currently plans to include outpatient (and inpatient) lower extremity joint replacement and spinal fusion, and the model may seek to expand to other conditions over time.
These two studies offer important messages for hospitals and clinicians participating in the TEAM model, as well as Medicare and other payers who continue to innovate with bundled payments. First, bundled payments should seek to align hospitals and physicians regardless of who is designated as the accountable provider. Second, outpatient surgeries may benefit from bundled payment approaches and should be tested in future models.
Through its mandatory design, TEAM offers an excellent opportunity to answer these questions and many additional important challenges, including the role of patient selection in contributing to model savings as well as changes in access or outcomes from surgery for historically marginalized populations. In the midst of major policy disruptions across the healthcare system, national experimentation with bundled payments will continue, as we stay in search of better ways to improve the quality of episodic care.
The study “Physician and Hospital Performance in Medicare’s Updated Bundled-Payment Model for Joint Replacement” was published in JAMA Health Forum on July 25, 2025. The authors include Aidan P. Crowley, Austin S. Kilaru, Qian (Erin) Hu, Erkuan Wang, Jingsan Zhu, Ayush Arora, Torrey Shirk, Deborah S. Cousins, Kristin A. Linn, Said A. Ibrahim, Joshua M. Liao, and Amol S. Navathe.
The study “Savings Associated With Bundled Payments for Outpatient Spine Surgery Among Medicare Beneficiaries” was published in JAMA Health Forum on July 11, 2025. The authors include Austin S. Kilaru, Grace Y. Ng, Erkuan Wang, Erin Huang, Aidan P. Crowley, Jingsan Zhu, Joshua M. Liao, Said Ibrahim, Torrey Shirk, Deborah S. Cousins, Neil R. Malhotra, and Amol S. Navathe.




New Study From LDI and MD Anderson Finds That Black and Low-Income, Dually Eligible Medicare Patients Are Among the Most Neglected in Cancer Care

Her Transitional Care Model Shows How Nurse-Led Care Can Keep Older Adults Out of the Hospital and Change Care Worldwide

Chart of the Day: Medicare-Medicaid Plans—Created to Streamline Care for Dually Eligible Individuals—Failed to Increase Medicaid Participation in High-Poverty Communities

Penn LDI Debates the Pros and Cons of Payment Reform

Direct-to-Consumer Alzheimer’s Tests Risk False Positives, Privacy Breaches, and Discrimination, LDI Fellow Warns, While Lacking Strong Accuracy and Much More

One of the Authors, Penn’s Kevin B. Johnson, Explains the Principles It Sets Out