
ED Psychiatric Boarding of Children Worsens Nationwide
Penn LDI Senior Fellow Dominic Sisti Cites “Alarming Levels”
Blog Post

Hospitals around the world confront the same hard truth: clinician burnout and turnover are not just workforce problems. They are patient safety problems.
For years, solutions focused on helping individual clinicians with approaches like resilience training, mindfulness initiatives, or workshops to support coping. But those supports leave the underlying system untouched. What if the most effective lever is not asking clinicians to adapt to broken conditions, but changing the system itself?
A new Medical Care study evaluates Magnet4Europe, a large-scale intervention involving 56 hospitals in six European countries, paired with U.S. Magnet hospitals to adapt the Magnet framework for workplace excellence. The results suggest that organizational change can improve clinician well-being and patient safety.
Magnet4Europe is not a single hospital success story. This coordinated effort spanned Belgium, England, Germany, Ireland, Norway, and Sweden. European hospitals were “twinned” with 65 U.S. Magnet hospitals, including all six Penn Medicine hospitals, to encourage mentoring and shared learning. A prospective study measured organizational changes in hospitals, and whether those shifts came with improved clinician well-being and patient safety. Magnet4Europe was designed and led by the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing in collaboration with KU Leuven in Belgium.
The timing makes the results even more striking. The project launched in early 2020 as COVID-19 swept across health systems. The intervention had to shift to virtual learning and remote mentoring during the first 18 months because of travel bans and disruptions. Even under extreme strain, participating hospitals sustained improvements in culture and practice.
A key strength of the study is that it did not treat “implementation” as a vague concept. Hospitals tracked progress using 77 Magnet model intervention targets, measured at baseline and follow up. They used a structured gap analysis tool – comparing an organization’s current state with its desired future one — adapted with permission from the American Nurses Credentialing Center.
These targets reflect the features that shape daily clinical work: leadership accessibility, clinician participation in decision-making, strong nurse-physician relationships, evidence-based practice, and using outcomes data to guide care improvement.
This is why Magnet is often described as a framework for building a work environment that supports professional practice. It focuses on how hospitals are organized, how decisions are made, and whether systems can learn from outcomes.
The study’s central question was straightforward. When hospitals adopt more of the intervention, do outcomes improve more?
They did.
Hospitals that improved implementation by more than 25 percent saw meaningful gains across multiple outcomes:
Moreover, improved nurse work environments led to reduced physician burnout and intent to leave, showing the importance of nurse wellbeing to that of other clinicians in hospitals.
The average European hospital, supported by its U.S. Magnet twinning partner, fully embraced about half of the Magnet features within two years.
For system leaders, these are not abstract differences. A reduction in intent to leave signals improved retention, workforce stability, and continuity of care. Improvements in quality and safety reflect day-to-day conditions that affect patients.
Hospitals that joined the Magnet4Europe experiment were already interested in improving clinician outcomes which made them open to adoption of best practices. Otherwise, they did not differ from other hospitals. Improvements occurred in hospitals regardless of country context and policies.
While the findings are compelling, we note that participating hospitals were volunteers and thus committed to change. Our measure of intervention implementation was detailed and showed variation by hospital. We cannot rule out that improved outcomes were related in part to unmeasured factors such as post pandemic hospital recovery. However, improved outcomes were directly associated with the extent of intervention implementation, and not all hospitals experienced improved outcomes over time bolstering the case that the intervention was driving improvements in outcomes.
Improvements occurred in hospitals regardless of hospital characteristics such as size and teaching status and country context and policies.
Clinician burnout and related turnover is widely recognized as a crisis, and workforce shortages make care less safe and harder to get. Yet large-scale evidence on what improves retention has been limited, especially when it comes to broader interventions.
This study helps fill that gap. It adds prospective evidence that the Magnet model is not simply a label that rewards high-performing hospitals but can shape work environments and outcomes.
The paper also points to a persistent challenge in the burnout response landscape: most interventions still focus on helping clinicians cope, rather than improving the systems where clinicians practice.
Magnet4Europe takes the opposite approach. It treats clinician well-being, retention, and patient safety as outcomes that can be improved through leadership, clinician empowerment, and evidence-based redesign.
If there is a single message, it is that clinician burnout is not inevitable, and retention is not solely driven by external labor markets. Work environments can be redesigned, and leadership choices matter.
Magnet4Europe offers health systems a practical playbook: invest in structures that empower clinicians, support evidence-based practice, and use outcomes data to drive improvement. The results suggest that these changes can translate into better clinician well-being and safer care, even under the most challenging circumstances.
The study, “Magnet4Europe Intervention to Improve Clinician and Patient Well-Being: A Quasi-Experimental Study of 56 Hospitals in 6 European Countries,” was published in Medical Care on December 22, 2025. Authors include Linda H. Aiken, Walter Sermeus, Karen B. Lasater, Reinhard Busse, Martin McKee, Herbert Smith, Jonathan Drennan, Claudia B. Maier, Jane Ball, Simon Dello, Dorothea Kohnen, Rikard Lindqvist, Anners Lerdal, Peter Griffiths, Wilmar B. Schaufeli, Hans De Witte, Lars E. Eriksson, Anne Marie Rafferty, Julia Köppen, Lisa Smeds Alenius, and Matthew D. McHugh.



Penn LDI Senior Fellow Dominic Sisti Cites “Alarming Levels”

Chart of the Day: Methadone Use for Opioid Use Disorder Tripled From 2010–2020, Yet Only One in Four People With Addiction Receive Medication
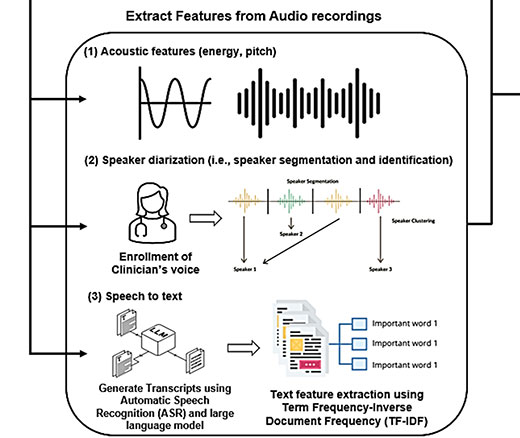
Researchers Use AI to Analyze Patient Phone Calls for Vocal Cues Predicting Palliative Care Acceptance

Medicare’s Payment Plan Can Ease Seniors’ Crushing Drug Costs but Medicare Buries it in the Fine Print

LDI Fellows’ Research Quantifies the Effects of High Health Care Costs for Consumers and Shines Light on Several Drivers of High U.S. Health Care Costs

Comment: Submitted to Centers for Medicare & Medicaid Services