Health Care Access & Coverage
News
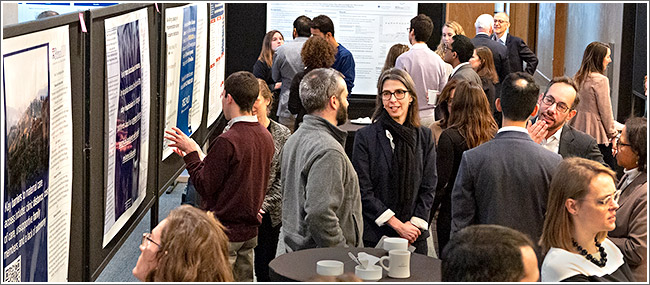
Photo Report From The LDI Health Policy Retreat 2020
Eighteen HSR Experts Discuss Their Latest Research As The Affordable Care Act Marks Its 10th Anniversary
 |
||
| Photos: Hoag Levins
Enhancing interdisciplinary discussion at this year’s Leonard Davis Institute of Health Economics’ Health Policy Retreat, was the addition of a poster session (above) featuring 20 research displays. The one-day annual retreat, originally founded in 2011 to foster cross-campus interaction and collaboration among University of Pennsylvania health services researchers, was held in the conference hall of The Study at University City. (Click image for larger) As the Affordable Care Act reached the 10th anniversary of its passage, the 2020 LDI Health Policy Retreat featured presentations by 18 experts in health care areas related to aging, vulnerable populations, access and coverage, and opioids. The thought-provoking research topics ranged widely — from physicians’ willingness to cooperate with new Medicaid work requirements in several states, to high nursing turnover in the home care industry; and from the effect of assumed criminality on pain prescribing for African American patients to the epidemiology of fatal and non-fatal firearm injuries. |
||
   |
||
| LDI Executive Director Rachel Werner, MD, PhD (above, left), welcomed attendees to the eighth annual LDI Health Policy Retreat for updates and discussions on the latest developments and trends in the field of health policy research. Above, right, moderated by Judith Long, MD, Chief of the Division of General Internal Medicine at Penn Medicine and an LDI Senior Fellow (above, left), the first panel focused on research projects related to health care in vulnerable populations. LDI Senior Fellow Damon Centola, PhD (hand extended), Director of the Network Dynamics Group at Penn’s Annenberg School for Communication, gave a presentation titled “Physician Network Intervention to Reduce Implicit Race/Gender bias in Clinical management of chest pain.” His body of research work, looking at bias as a function of peoples’ social networks, is testing various network interventions to alter participants’ thinking and actions. In this instance, the target was the way clinicians’ treatment of African American female cardiac patients differs from the treatment of male patients. | ||
  |
||
| The “Public Health Epidemics: Opioids and Violence” panel was moderated by LDI Senior Fellow Zachary Meisel, MD, a Penn Medicine emergency physician and Director of the Center for Emergency Care Policy Research. “The two topics may not seem to overlap, but there’s actually a ton of overlap,” said Meisel. Speaking on a key element of the violence part — firearm injuries — was LDI Senior Fellow Elinore Kaufman, MD, MSHP, Fellow in Surgical Critical Care and Trauma Surgery. Studying the epidemiology of firearm injuries, she estimated there are 40,000 deaths and 82,000 non-fatal injuries related to firearms each year in the U.S. That’s 280 firearm injury incidents a day. Above, right, talking about the opioid part, was LDI Senior Fellow Douglas Wiebe, PhD, a Perelman School of Medicine Professor and Director of the Penn Injury Science Center (PISC). The Center’s researchers are working with the local nonprofit Safehouse to establish the country’s first Supervised Injection Facility (SIF) in Philadelphia — an effort the U.S. Justice Department seeks to block with a civil lawsuit. “We probably cannot stop the opioid epidemic in Philadelphia dead cold,” said Wiebe, “so we want to do harm reduction and create a facility where individuals can use injection drugs under supervision and in a safe way.” | ||
 |
||
| A highpoint of the retreat was an ACA lookback discussion by two leading experts on the topic: Ezekiel Emanuel and Robert Moffit. Emanuel, PhD, MD, MSc, Penn Vice Provost and former Obama White House consultant and an architect of the ACA, is also author of the 2015 book, Reinventing American Health Care: How the Affordable Care Act Will Improve our Terribly Complex, Blatantly Unjust, Outrageously Expensive, Grossly Inefficient, Error Prone System. Moffit, PhD, is a former senior Reagan Administration HHS official and currently a Senior Fellow at The Heritage Foundation conservative think tank. He authored the 2011 book, Why Obamacare is Wrong for America: How the New Health Care Law Drives Up Costs, Puts Government in Charge of Your Decisions, and Threatens Your Constitutional Rights. | ||
  |
||
| Penn Nursing School Assistant Professor and LDI Senior Fellow Karen Lasater, PhD, RN (above, left), detailed her project using an algorithmic patient matching approach to create an approximated randomized control trial to analyze how different nursing environments affect patient outcomes, costs of care. The algorithm was designed to identify pairs of patients from among 300,000 Medicare fee-for-service patients. To pair, two patients had to be as similar as possible in 40 different clinical and demographic variables. One patient in the pair went to a hospital with better nursing resources, the other was in a hospital with worse nursing resources. “We found that patients who attended the better nursing-resourced hospitals had significantly lower mortality than their matched pair,” said Lasater. “We also found that they had a slightly higher cost — the difference being about $840 in an overall cost of about $20,000.”
Above, right, Health economist Alon Bergman, PhD, discussed his study of the high turnover of nurses in home care. He is a Postdoctoral Researcher at LDI and The Wharton School and an LDI Associate Fellow. His team worked with HR data from one of the country’s largest home care companies that experiences an annual turnover rate of 22%. He cited the volatility of scheduling as a key factor. Home care nurses have little control over scheduling, which is assigned by the branch office. They have no input into that process and are not aware of their schedule until the night before. “This plays to play a significant role in their decisions to quit,” Bergman said. |
||
  |
||
| Shoshana Aronowitz, PhD, FNP-BC (above, left), a National Clinician Scholar at the Perelman School of Medicine and an LDI Associate Fellow, discussed her review study of racial disparities in pain treatment and the assumed criminality of African American patients. The latter belief makes some clinicians more likely to implement risk-reduction strategies, like urine screening or limited early refills, with black patients than white patients. Above, right, Harald Schmidt, PhD, MA, Assistant Professor of Medical Ethics and Health Policy at the Perelman School and LDI Senior Fellow, details his study of physicians’ attitudes and behavior related to their administration of Medicaid work requirements. The new rules in several states require patients to work between 80 and 100 hours a month in order to be eligible for Medicaid coverage. | ||
  |
||
| Events convened by LDI throughout the year are routinely designed to maximize audience engagement and this one was no different. Above, left, former CEO of the University of Pennsylvania Health System and LDI Senior Fellow Ralph Muller, MA, provides his insights on hospital management practices during a Q&A session. Above, right, David Grande, MD, MPA, Director of Policy at LDI and Associate Professor of Medicine at the Perelman School of Medicine discusses a point of national health policy politics. | ||
  |
||
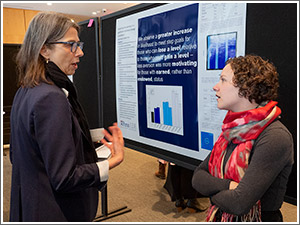
| At the retreat’s poster session (above, left) are Amelia Van Pelt, MPH, an LDI Associate Fellow and Doctoral Epidemiology Student in the Department of Biostatistics, Epidemiology and Informatics; Stephanie Mayne, PhD, MHS, and Assistant Professor at the Children’s Hospital of Philadelphia and an LDI Senior Fellow; and Salama Freed, PhD, MA, MS, a Postdoctoral researcher at LDI and the Department of Medical Ethics and Health Policy. The poster is of a Mayne study published in the Journal of Urban Health that found women living in neighborhoods with higher levels of physical disorder had a higher risk of adverse birth outcomes.
Above, right, discussing an evaluation of loss aversion in a gamification behavior change intervention is Judith Long, MD, Chief of the Division of General Internal Medicine at Penn Medicine and an LDI Senior Fellow, and Ashley Ritter, PhD, CRNP, a Penn School of Nursing Postdoctoral Fellow, MSHP Student, and LDI Associate Fellow. |
||
  |
||
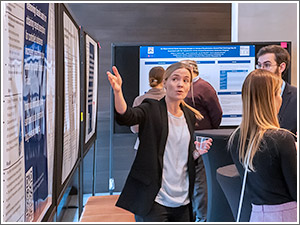
| Above, left, Katharine Rendle, PhD, MSW, MPH, explains her poster about a study of annual lung cancer screening programs for high-risk adults at two major medical centers. She is an LDI Senior Fellow and Director of Implementation Science at the new Penn Center for Cancer Care Innovation (PC3I). Above, right, Associate LDI Fellow and Postdoctoral Researcher at LDI Liisa Laine, PhD, MSc, explains her poster project to Jeffrey Lienert, PhD, an Advanced Fellow in the Penn Center for Health Care Innovation’s Nudge Unit. | ||
  |
||
| Guy David, PhD (above, left), LDI Senior Fellow and Professor of both Health Care Management at The Wharton School and Medicine at the Perelman School of Medicine, was moderator of the “Coverage and Delivery” panel. Above, right, panelist Matthew Grennan, PhD, Assistant Professor of Health Care Management at The Wharton School and LDI Senior Fellow, spoke about his body of work related to the variation in prices for medical devices and services. “In the last few years, due to some great work by organizations like the Health Care Cost Institute, ECRI and others, we’ve had the opportunity to get a window into what’s happening in terms of the prices and dollars being exchanged in the private health insurance market,” Grennan said. He cited wide variation in prices for things like knee replacement. Some hospitals charge $35,000 for the procedure while others charge $15,000 for the same operation. Prices for the actual knee replacement device vary equally widely — from $5,500 in some hospitals to under $1,000 in others. Grennan noted that those knee device costs are for “the exact same device from the same vendor at the same point in time.” | ||
  |
||
| A mid-day “Successfully Pitching Your Research” session brought in Dan Gorenstein (above, left), long-time journalist and former Senior Health Reporter on American Public Media’s radio show Marketplace, to help researchers hone their media skills. Gorenstein, an LDI Adjunct Senior Fellow, is now Executive Editor and Host of the Tradeoffs podcast, produced in collaboration with LDI, the Annenberg School for Communication and Penn’s Center for Public Health Initiatives. Members of the audience, like Rinad Beidas, PhD, Director of the Penn Implementation Science Center (PISCE), came up on stage to ‘Pitch the podcaster.” Her suggestion was a news feature focused on the little-appreciated fact that half of all suicides are accomplished by gun — and that storing guns more safely in the home would reduce suicides. Above, right, Alison Buttenheim, PhD, MBA, LDI Senior Fellow and expert in school vaccine exemption policies, talked through her recent pitch to Pennsylvania state Senator Daylin Leach (D-Delaware & Montgomery counties). Leach was preparing new legislative proposals to further tighten state exemption policies. | ||
  |
||
| Chatting during a break (above, left) were Ezekiel Emanuel, Roy Rosin, MBA, Penn Medicine Chief Innovation Officer, and Courtney Schreiber, MD, MPH, Chief of the Penn Medicine Division of Family Planning and an LDI Senior Fellow. Above, right, Rinad Beidas with Rebecka Rosenquist, MSc, Health Policy Director at the Policy Lab at Children’s Hospital of Philadelphia. | ||